Contents
1. Introduction
1.1 Safeguarding Adults Review (SAR) referrals with concerns about failure of agencies to work together were received by Torbay and Devon Safeguarding Adults Partnership (TDSAP), for three men who died during the pandemic in the Devon area. A thematic review model was agreed to identify and share learning to improve future interagency practice and prevent deaths or serious harm in similar circumstances.
1.2 The men were aged 59, 53, and 46 years. Whilst the three men had different individual circumstances, there were parallel themes. Their mental health and associated difficulties were complex, with escalating distress and requests for help.
2. SAR process and methodology
2.1 This review was a statutory learning-focused process. The aim was not to re-investigate, but to evaluate and explain professional practice, highlighting challenges, system problems and constraints to practitioner efforts to safeguard adults. Interagency working, and insight into improving responses to men in similar situations are encompassed within the analysis and findings. Case detail required exploration to understand the circumstances and consider potential themes. The Social Care Institute for Excellence (SCiE) Safeguarding Adults Review[1] Quality Markers (QMs)[2] were used in this review as evidence of SAR governance and to demonstrate transparency. See Appendix 6
| Empowerment | Understanding how individuals or representatives were involved in their care.
|
| Prevention | The learning will be used to consider how practice can be developed to prevent future harm to others. |
| Proportionality | The learning from three cases will be more effective in considering systems and if themes are repeated in other cases. |
| Protection | The learning will be used to protect others from harm. |
| Partnership | Partners will cooperate with the review considering how partners are working together to safeguard adults. |
| Accountability | Agencies will be transparent in the review with the TDSAP holding individual agencies to account for agreed recommendations. |
2.2 The Department of Health’s (DoH) six principles for adult safeguarding are included in this review as described below. These are principles that should be applied across all safeguarding activity[3].
2.3 The Terms of Reference were drawn up and confirmed in June 2022, see Appendix 1. The areas centre on the wider context of working with individuals with complex mental health needs, self-harm, and consideration of services from the perspective of trauma informed. The structure of the report is divided into the domains used in the analysis of SARs 2017 – 2019.[4] 1. Direct work with individual(s), 2. Inter-professional and Interagency collaboration, 3. Organisational features of the agencies involved affecting how practitioners and teams worked, 4. SAB leadership, oversight, and governance.
2.4 Decisions were made by TDSAP in conjunction with the Lead Reviewer (LR) about the wider contextual factors, the need to find the right balanced approach, and one that included proportional methodological rigor. There was acknowledgment this review was delayed. Factors impacting on the timeliness of this SAR were highlighted as the pandemic, agency capacity and delay finding an independent LR with the right background and experience. See Appendix 8 for the LR’s biography.
2.5 Agencies provided their internal Management Reviews (IMRs), and from these a multi-agency chronology of events for each man was produced. The chronologies generated key events (KE) and questions, see footnotes in chronologies Appendix 2,3, and 4. These identified that supplementary information was needed to clarify facts, and explore questions. Unfortunately, there were obstacles in gaining more information.
2.6 There were parallel processes for coroner inquests, held in June and July 2021 and January 2023. The coroner witness statements for all three deaths were provided to the SAR. Mental health policies and operating procedures were provided in November and late December 2022. The LR also spoke with the coroner and attended an inquest via video in January 2023.
2.7 As a result of the difficulties experienced, the planned collaborative systems model with relevant staff was not possible, therefore, to compensate, a blended review model[5] was used. This included a combination of IMRs, and interviews with available relevant staff and family members, see Appendix 7. Perspectives of individuals, families and organisations were included from IMRs, and inquest witness statements. The latter was also used to offset the inability to access additional information.
2.8 Relatives of one man did not want involvement, and friends of another could not be located. The third man’s family did not want to engage with the review, and in a telephone discussion, requested an opportunity to consider findings after the inquest. Late in the process the LR identified another relative. A TDSAP representative made enquiries ensuring there was an opportunity for all relevant family to be involved. The next of kin of one man who participated in the review, raised other matters, requesting answers to broader questions about the mental health care. Disappointingly it was not possible to address these in this review due to the inability of mental health services to provide additional information. These questions will now be addressed in a meeting with the family and the relevant clinical team.
2.9 The analysis, findings and themes identified in this SAR will be taken forward by TDSAP and shared with family and agencies involved.
[1] Section 44 (1-3), Care Action 2014
[2] SCiE Safeguarding Adults Review Quality Markers. Comprehensive checklist tool March 2022 – https://www.scie.org.uk/files/safeguarding/adults/reviews/quality-markers/scie-sar-quality-markers-comprehensive-checklist.pdf
[3] Department of Health (2016 Care and Support Statutory Guidance Issues under the Care Act 2014)
[4] Local Government Association ‘Analysis of Safeguarding Adults Reviews (SARs April 2017 – March 2019). https://www.local.gov.uk/sites/default/files/documents/National%20SAR%20Analysis%20Final%20Report%20WEB.pdf
[5] from the Torbay and Devon Safeguarding Adults Partnership SAR decision and methodology tree.
3. The men – circumstances of death and personal histories
3.1 The deaths included in this thematic SAR are as follows,
NB, there was limited information available for Adult N, available to this SAR.
3.2 ADULT C
Adult C, aged 59 and white British, died on 4th September 2020. The inquest was held in July 2021. The medical cause of death has been ascertained as multiple injuries due to a fall from height and the Inquest recorded an outcome of suicide, “that it is more likely than not that C intended to take his own life that day”. Adult C jumped from cliffs in Devon, at 18:50pm. At the time he was separated, unemployed, experiencing mental health difficulties and living in supported accommodation. Police received a call from care staff at 13:57, reporting that he had again left the accommodation, there were concerns about mental health and wellbeing. Police began a search and later Adult C was seen, he had fallen halfway down the cliff. A suicide note and a bag containing possessions were found at the top of the cliff. Despite efforts by a lifeboat crew to verbally engage with him, Adult C made his way further to a steeper area and then dropped from the cliff approximately 150 feet sustaining fatal injuries.
3.3 ADULT N
Adult N, aged 53, and white British, died on 11th September 2020. The inquest was held in January 2023. The autopsy recorded a cause of death as asphyxia due to hanging. At the inquest the coroner recorded a narrative conclusion, “at the time of death Adult N was experiencing mental health difficulties……He died as a consequence of his own actions. There was insufficient evidence to conclude this was a planned deliberate act as it was not clear what his intentions were”. The coroner commented that it was possible Adult N was unaware how quickly he would experience difficulty. Prior to death Adult N had a decline in his mental health with multiple ambulance attendances over a five-week period for impulsive overdoses while under the influence of alcohol. Referrals were made to the liaison psychiatry team at the Emergency Department (ED). On the morning of death sometime before 06.00 hrs, he woke his mother asking her if she would like a cup of tea. After about thirty minutes later his mother saw he was suspended, hanging from a banister spindle by a dressing gown cord around his neck. His mother called 999. On the paramedic’s arrival there was no respiratory effort and no cardiac output. Police were contacted and attended, his room was checked and two large 2-litre bottles of cider, one empty and the other three quarters empty, were found. The post-mortem established that Adult N was not intoxicated at the time of his death, nor had he taken any drug in high dosage.
3.4 ADULT B
Adult B, aged 46 and white British, died on 19th January 2021. The inquest was held in July 2021 and the outcome was recorded as suicide; and on the balance of probability, it was an action he intended…“it appears that B jumped off the roof terrace of the building in which he lived. There was nothing to suggest anyone else was involved in his death. It is likely that the fall from this height caused him to become unconscious and he came to rest in a position where breathing was not possible, a set of situations known as positional asphyxia. In the absence of other findings, it is reasonable to attribute death to this”. Adult B is described as having a number of mental health diagnosis and a mild to moderate learning disability or difficulty. Adult B was described as mentally unwell and distressed prior to death. Staff at the accommodation last saw him the previous evening. On the morning of 19th January 2021, staff went to his flat and found him missing. Adult B had left shoes and clothes on the floor; his mobile was also found, all which staff thought was unusual, and he was reported missing to police. Following a search of the building he was located at 09:25 am on the ground at the rear of the building. Staff commenced resuscitation attempts but this was not successful, and Adult B was pronounced dead by the ambulance crew shortly after.
4. Adult C background information – pen picture of adult C
4.1 This information is provided with the kind assistance from Adult C’s eldest daughter. Loving memories of her father were shared with this review so the LR and those reading this report could know how he was as a man and a father, when he was well, allowing Adult C to be held at the centre of this themed review.
4.2 Adult C was a much-loved father to three children, as well as stepfather to three from his third marriage, and was a new grandfather to one. Adult C and his eldest daughter shared the same birthday and there was a special bond. The dad his children will always remember was awkwardly funny, extremely caring, and easy to wind up. He was calm, evenly tempered, and super organised. He was a fantastic father. He was especially skilled at DIY and kept the family home in top shape. He enjoyed mowing the grass and was proud of his garden. He was a keen driver and throughout his life drove a range of cars, buses, quadbikes, lorries, and tractors. He loved animals, and although he protested, he enjoyed looking after the many family pets, including hamsters, guinea pigs, rabbits, and cats.
4.3 For much of his adult life Adult C lived in the Southwest, although he grew up in Buckinghamshire. He was born in Chorley Wood and was the youngest child to his parents, and a brother to his sister. After leaving school, which is where he met the mother of his three children, he worked on various farms, mainly as a tractor driver. He loved working in the fields and being on the land. After working in agriculture in his early career he then worked for a local bus company driving school buses, he especially enjoyed taking children on school trips. The family then moved to Devon, after making the decision to move following a family holiday to the seaside, and he worked for many years for Southwest Water in their treatment plant. Here he worked shifts, but this did mean that he enjoyed 11 days on and 11 days off, which he could spend with the family. His family reflect on many happy memories spent during the school summer holidays at the beach, they had a beach hut and would spend long days splashing in and out of the water, he would pull the children along in rubber rings. He always joined in with games and made them laugh a lot. He worked hard to take them on family holidays and was a professional at packing the car without even a centimetre to spare. Once settled in Devon he maintained his friendships in Buckinghamshire with two families, who became honorary Aunties and Uncles to his children. One family even moved to joined them in Devon and moved across the road. He would enjoy many an evening BBQing and cooking up a feast for his friends and family. He collected Toby Jugs and stamps, meticulously organising them.
4.4 Later on in his working life he went on to work as a delivery driver, he volunteered in a British Heart Foundation charity shop and began training to become a driving instructor, unfortunately his mental health meant that he didn’t ever finish that qualification. When his health was good, he was a keen runner, especially enjoying jogging along the seafront. He also played table tennis and joined a local club. He loved the band Queen and would listen to them; he took his daughter to a Queen tribute band for her eighteenth birthday, which to this day is one of her fondest memories of her father. He also loved action type films, especially James Bond and he supported Arsenal Football Club. When his children were growing up, he got hooked on playing Crash Bandicoot (a game he bought for them) on the PlayStation and was even caught playing it when they had gone to bed.
4.5 Adult C suffered with his mental health for nearly 20 years prior to his death. During this time, he suffered peaks and troughs, although even in his better times he never returned to the man he once was. When mentally more stable he was able to rebuild his life, doing voluntary work and gaining employment. In the periods of more stability, he made new relationships and married twice more, although his levels of anxiety and fear impacted on relationships with all family members and friends. Despite at times being very unwell, his family was always at the forefront of his mind and never stopped being his priority. Adult C was 59 years old and three days short of his 60th birthday at the time of his death.
4.6 Social circumstances
Adult C was married three times, most recently in May 2018, and separated in August 2019. Adult C had limited contact with his three adult children, although had telephone calls with his eldest daughter. Supported accommodation with care staff was agreed in the spring of 2020, and he moved into a five bedroomed house with four other residents.
4.7 Employment
Adult C worked in a variety of jobs, in agricultural work, and for Southwest Water and more recently as a logistics delivery driver and appliance installer. Due to the deterioration in his mental health, he had not been employed for some time.
4.8 Care and Support needs
Adult C had a range of care and support needs, these are described as health, mental health, and adult social care needs. The latter included supported accommodation (also known as extra care housing), additional enabling one to one hours on top of core hours at the accommodation for leisure and occupation, prompting of activities of daily living, review, and monitoring of medication for mental health and support to help him minimise harmful alcohol consumption.
4.9 Physical health history
Adult C had physical health care for back pain and a brain scan in 2017. The scan showed evidence of a stroke. A repeat scan in May 2020 showed some evidence of the earlier stroke, but there was no significant change from the 2017 scan. Adult C had a history of excess alcohol use and oesophagitis. In November 2019, he was an inpatient in the District General Hospital (DGH) where he received care for physical health problems related to alcohol detoxification.
4.10 Mental Health history
Between 2001 to 2004, Adult C had at least seven admissions to an acute adult mental health inpatient unit after deterioration of his mental state and suicidal thoughts with intent, i.e., going to the cliffs, constructing a noose in the loft and acts of self-harm. The admissions were both formal under the Mental Health Act (MHA) and informal. His diagnosis was treatment resistant depression, and his presentation was described as complex. Adult C had a course of Electro Convulsive Therapy[6] (ECT) for agitated depression in 2005. During this period his first marriage broke down. Adult C also had long term psychotherapy, family and drama therapy. The psychotherapy was aimed at changing the way he thought and behaved to improve his mental and emotional wellbeing. Family reported that he recovered well. Clinicians noted that Adult C had difficulty in thinking about his problems and behaviours from a psychological perspective and engaging with therapy, and he also struggled to consistently take medication. There was no contact with mental health services after 2005 until April 2017, when Adult C experienced low mood and agitation. The contributory factors included employment worries, an injury resulting in back pain, and sleep disturbance. Adult C declined medication for pain and the GP referred him to mental health services.
4.11 During 2017 there was a significant deterioration in his mental health, and he received daily care from the Crisis Resolution Home Treatment team (CRHTT). Significant events included his pacing around the home all night, he was described as if someone had switched the off button on his brain and he wasn’t there anymore, and it was weeks before he calmed down. His partner found this frightening. A range of medication was tried but he was reluctant to take this. Staff who knew Adult C from earlier mental health care, noted his presentation was similar to previous hospital admissions. Severe depression and anxiety were diagnosed and after discharge from CRHTT, he received support from the community mental health team (CMHT), with a care coordinator, firstly with home visits and later he attended at the office base. Care included medication, talking and self-help books. Adult C repeatedly asked to be admitted to hospital to ‘fix him’. A range of medication was tried, and as soon as one was working, he believed this was not the one for him, and every time medication changed the suicidal thoughts started again. In October 2017, Adult C’s mental health deteriorated again, and he was referred to the CRHTT with depressive symptoms and suicidal thoughts. He was refusing medication and found with a belt around his neck pulled tight, he said he wanted to kill himself, after this Adult C was admitted to an older person’s ward. It was noted that each time medication was started, he would feel better, but could not accept he was suffering from anxiety and depression, and he stopped taking medication. When discharged he was prescribed antidepressant and antipsychotic medication. A brain scan was agreed to try and provide some reassurance that there was nothing wrong with his brain, which was a feature of his anxieties. From November 2017 – November 2018, Adult C was supported by the CMHT and discharged when he was doing well. After discharge Adult C wanted to change his medication. This pattern of distress continued over the next two years.
4.12 Since November 2018 Adult C’s distress continued, with his partner as his full-time carer. Adult C was encouraged to attend activities during the day, he attended for a while and then refused. He was described as starting the day in panic, so he kept busy, which took his mind off his illness, and the next day it started all over again and he was not able to deal with everyday life. In December 2018 the GP referred Adult C to mental health services with low mood, anxiety, and an inability to cope. Nothing had changed in two years and Adult C needed more support, CHRTT then provided care. In July 2019 the carer arrangements broke down, he was too dependent and described as childlike. Adult C then stayed with his eldest daughter for a few days. His anxiety was described as ‘through the roof’, and he was constantly pacing. He repeated phrases, that his mind was not working, and that he was broken continuously. His daughter was worried about leaving him alone for fear of what he might do. When he returned home in August 2019, his relationship was over. CRHTT provided support, and respite accommodation with care staff was arranged for a few weeks. Adult C continued his refusal to cooperate with mental health care and treatment. He was then re-referred to community mental health services by his GP with low mood and memory problems, and he was taken onto the caseload of the local CMHT. Later visits to his daughter to meet his new grandchild in 2019 saw Adult C’s behaviour as centred around his anxieties, he was acutely unwell with anxiety and agitation.
4.13 Forensic history / Police involvement
Adult C was known to police due to concerns about his mental health, he did not have any convictions, recorded cautions, or warnings. From October 2019 until death, police had eleven contacts with Adult C in connection with his mental health crisis, suicidal thoughts, threats to jump from the cliffs, threats to harm himself with a knife, and as a high-risk missing person.
4.14 Agencies involved
The agencies involved in Adult C’s care were GP services, mental Health Service, Mental health social worker, Respite supported living, Enabling Support, accommodation with supported Living, Police, and the ambulance service.
[6] ECT is a treatment that involves sending an electric current through your brain, causing a brief surge of electrical activity within your brain (also known as a seizure). The aim of the treatment is to relieve the symptoms of some mental health problems.is an effective treatment most commonly used for severe depression that hasn’t responded to other treatments. It is usually considered when other treatment options, such as psychotherapy or medication, have not been successful or when someone is very unwell and needs urgent treatment.
5. Adult N background information – pen picture
Biographical information available to the SAR for Adult N from all agencies was limited. Adult N was a 53-year-old man who lived with his mother for whom he was the main carer. Adult N had supportive neighbours and felt able to knock on their door seeking support for anxiety a few weeks prior to his death. The neighbour is described as a good friend to the family, and a lifelong friend from his schooldays. Adult N’s father passed away in 2002. He was described by his mother as a kind and even-tempered man, and both got on well with each other.
5.1 Adult N was described as very good at looking after his mother. His mother was concerned about his drinking, and she tried to stop it, as she controlled most of the household budget. His mother explained he would ask for money, and if this was not forth coming, he would threaten to ask family, friends, or neighbours. His mother would have felt very embarrassed about this, so she gave him the funds.
5.2 Social circumstances
Adult N was described as not particularly academic at school. He married around 2003 and went to live in Newton Abbot with his wife, but sadly the marriage only lasted a few years before they separated, although they were married for sixteen years. There were no children and Adult N later moved back to the family home with his mother. His wife continues to live in the same county, and details of their relationship at the time of death is not known. He was in receipt of Employment Support Allowance (ESA),[7] due to struggling with his mental health. In the weeks prior to his death, he described anxieties and worries related to his mother and the pandemic.
5.3 Employment
After Adult N left secondary school, he began working with his father who was an electrician with a local firm. He was taken on full time by the company and then later moved on to another business in the same line of work. Adult N then changed his employment and started working at a local business unit cooking food. After this he went on to become a carer at a care home, mainly working the nightshift, for four or five years. Unfortunately, poor attendance due to sickness led to the end of this employment. Adult N had not worked for thirteen years, his last employment was in a mental health provider as a health care assistant. There are no details as to whether Adult N received the ESA benefit on the criteria of unable to work or, that he was able to work and in receipt of help to return to work.
5.4 Care and Support needs
Adult N’s care and support needs were described as mental health, anxiety, and depression, which was impacted by excess alcohol. The GP prescribed medication for anxiety, depression, and insomnia. Adult N used self-care techniques and general lifestyle changes with the aim of managing symptoms of anxiety and depression, and to prevent deterioration.
5.5 Physical health history
In 2019 the GP was consulted about lower back pain with advice for self-referral to the NHS physiotherapy team and advice given for exercise and lifestyle. There was no other information of note related to physical health history.
5.6 Mental Health history
Adult N was very close to his grandmother who lived with them, and he was very upset when she passed away in the late 1980’s. His mother believed this may have been a trigger for a deterioration in his mental health, as he suffered a breakdown which resulted in treatment at a mental health Unit in Torquay. There was a long history of mental health problems. He was initially diagnosed with severe anxiety and a possible psychotic episode in 1993 where he was admitted to hospital. He had been working in a nursing home at this point, was very stressed at work and he went through a marital breakdown. The GP records show that Adult N had a further episode of anxiety where he required psychiatric input in 2008 and he accessed talking therapies. There was a further episode of depression and there were referrals for talking therapies in 2010, 2012, 2014 and 2017. In August 2020 his GP again referred him to depression and anxiety services.
5.7 In December 2017 Adult N was taken to the ED at the General Hospital after a fall. Here he disclosed a history of depression, anxiety, suicidal thoughts, with some obsessional thinking which he saw as obsessive-compulsive disorder (OCD)[8]. Adult N disclosed he was drinking daily (two bottles of wine and some whiskey) to ‘block out’ negative thoughts, this was described by him as ‘on and off. Adult N described difficulty sleeping and an inability to gain pleasure from his usual activities such as music and gardening. His mother recalled Adult N had episodes where he went to neighbours houses uninvited to see how they were, or introduced himself as if they weren’t known to them. On occasion he would take his mother along, who felt she should go with him so she could explain and make sure he didn’t say anything untoward or upset people. It seemed at times, he felt he needed over extended contact to make a connection with people, and this could be uncomfortable for the neighbours. Adult N made excuses to check unnecessary small details again and again with people if they were going out or if they were doing a favour for him.
5.8 Since the pandemic lockdown, Adult Ns mental wellbeing deteriorated. He began to drink an excessive amount and was buying two litre bottles of cider from the nearby store. Sometimes this might be two to four bottles a day and he drank them downstairs in the kitchen, but also would have cider in his bedroom. In addition, shortly before his death, he disclosed drinking larger quantities of alcohol (9 litres of cider) each day, starting when he got up in the morning. Adult N was described as never appearing to be physically drunk, in the sense of losing his ability to function, so it was difficult to know exactly how much he had consumed. The neighbour recalled that he sometimes appeared a bit confused when they talked and seemed more anxious recently.
5.9 Agencies involved
The agencies involved in Adult Ns care were the Emergency Department at local general hospital, mental health services – First Response Service (FRS) and Liaison psychiatry (LP), locally commissioned talking therapies, GP, Drug and alcohol service, and the ambulance service.
5.10 Forensic history / Police involvement
None known.
[7] ESA – Employment and Support Allowance (ESA) is type of benefit. It is to help those who are affected by a health condition or disability. Furthermore, their condition must make them less or not able to work. When earning this benefit, people may get one of two things. First, if unable to work person will receive money to cover living costs. Second, you if able to work. Then, person will be provided with help to aid them in working again.
[8] Obsessive–compulsive disorder (OCD) is a mental and behavioural disorder in which an individual has intrusive thoughts (an obsession) and feels the need to perform certain routines (compulsions) repeatedly to relieve the distress caused by the obsession, to the extent where it impairs general function.
6. Adult B background information – pen picture of adult B
Adult B is described by the adult social worker, supported living staff and those who knew him as a considerate and kind man, who needed time to build relationships and time to communicate, and that he was often very distressed by intrusive thoughts. Adult B was also described as being protective of others and staff regarding his intrusive sexualised thoughts. This was illustrated by his looking away from and raising his voice at children when they visited the accommodation for Christmas carols. This was perceived as being a way of making sure the children did not have contact with him. Trust was a key contributory factor to whether Adult B would confide or share his thoughts, this was also believed to be a self-protective factor, for example, his concern about being judged by others or embarrassed by his thoughts. As his mental health deteriorated, he was observed to have difficulty in focusing on anything other than his thoughts and feelings, although he continued to engage with those supporting him, but in a minimal way. Adult B was also described as using self-isolation as a way of protecting himself and others due to his thoughts.
6.1 Biographical information available to the SAR for Adult B from all agencies was limited. It is recorded by various agencies that Adult B lived in Devon as a child, and both his parents were deceased. Adult B had a younger sister, from whom he was estranged, with no contact for over thirty years. His sister’s only contact was after death, where she helped the adult social worker clear the flat of personal belongings.
6.2 Adult B described his childhood as ‘not good’; he had difficult relationships with his parents, he described this as mainly related to his having learning difficulties and that his sister did not. Adult B disclosed he was physically abused by both his parents. He disclosed in addition to the physical abuse, he was also sexually abused by his father, a headmaster, and another pupil. Adult B also reported being bullied by others whilst at school. His age at the time of these allegations was not recorded. Police records include details of the emotional and physical abuse by his mother. This was described as his mother frequently hitting him with a rolling pin to the head and with her purse across his face. Adult B disclosed when distressed by intrusive thoughts, that he had sexually abused another young person when he was in his teens. Adult B left home when he was a teenager and presented himself to local services where he was placed into care. Adult B was given a place at a care home in Torquay, and he lived there from approximately 1993 to 2015. Subsequently in 2015 the manager, who had been a friend and carer to B for nearly 20 years moved, and B went with her to other accommodation in Torquay. It is not clear from records if this address was a care home, an adult placement or living with a friend.
6.3 Adult B attended school in Exeter which provided education and support to boys with emotional and behavioural difficulties.
6.4 The police were aware of the allegations of abuse Adult B had made against the headmaster but were unable to progress it any further due to a lack of corroborative evidence needed to bring a prosecution.
6.5 Social circumstances
Adult B had lived in care since he was a young person, and for the last twenty-two years with the same carer until 2018, when B was supported by an adult social worker (Torbay) to move. It is not clear what led to the breakdown of the care arrangements. The long-term carer only visited Adult B once after he moved into his new home, then there was no further contact, which he found distressing. Since May 2018, Adult B lived in extra care housing with care from supported living staff. The accommodation consisted of 29 one-bedroom flats and 16 two-bedroom flats with communal facilities for people normally over the age of 55 years with physical disabilities, mental health needs, older age, and dementia. Each apartment had a small kitchen, the local shop delivered groceries to the building in the morning, and there was also a restaurant providing breakfast and lunch. Staff were available and visited Adult B regularly as and when required throughout the day.
6.7 Employment
There was no detail about previous employment prior to the move to supported living. Since the move Adult B worked as a volunteer on a Monday and a Thursday at a charity shop in Torquay. He stopped volunteering when the shop closed during the pandemic. Adult B said he enjoyed working as a volunteer for the charity, recycling unwanted furniture to those in need. Adult B stated this gave him purpose.
6.8 Physical health history
Adult B was diagnosed with type 2 diabetes many years ago (date not recorded) and had diabetic retinopathy in both eyes which can cause blindness if left untreated. None of the information provided records the extent to which B’s eyesight was affected by this. In 2016, Adult B was diagnosed with hydronephrosis, which is a swelling of the kidney caused by a blockage in the urinary tract and he received treatment. In August 2019, B was admitted to the intensive care unit of the local DGH with a gastrointestinal bleed due to a duodenal ulcer. This was treated successfully. Alcohol use was disclosed by B in 2019 and a factor in this health condition. Adult B was on the GP learning disability register and had annual health checks at the surgery.
6.9 Care and Support needs
Adult B had long term mental health and care and support needs[9]. Adult B had mild learning difficulties which was also referred to as mild learning disabilities in information provided to the SAR. The adult social worker who knew him well described Adult B’s mental health was characterised by psychosis, obsessive thoughts and behaviour and low motivation. In October 2017 the care act assessment recorded his needs as requiring help with nutrition, personal hygiene, being appropriately clothed, maintaining his home, developing / maintaining family or personal relationships, accessing / engaging in work, and making use of community facilities. There was daily support in working hours from supported living staff at the accommodation with one member of staff on duty overnight.
6.10 Mental Health history
In 2008, Adult B was assessed by a learning disability clinical psychologist working within local adult mental health services in Devon.[10] The assessment concluded that Adult B was not eligible for an ongoing learning disability (LD) service due to the low level of impairment. This assessment outlined the view that his predominant need was mental health. Adult B’s first known contact with local adult mental health services was in October 2011 when he was given a differential diagnosis[11] of obsessive-compulsive disorder (OCD), mild learning disability, anxiety, mixed obsessive thoughts, and acts. Records also included developmental disorder – scholastic skills, which was unspecified, and paranoid schizophrenia.
6.11 Adult B is described as receiving a low level of support much like a befriending service rather than treatment from the CMHT until January 2016, when his mental health was recorded as stable, and his care was transferred back to his GP who was provided with medication advice.
6.12 In October 2017, Adult B was re-referred to local mental health services in Devon by his carer and her partner. There was a concern that Adult B’s mental health was deteriorating. Mental Health services recorded that the referral appeared to be a breakdown between Adult B and his carers rather than a specific mental health issue. It was concluded that he was not presenting with any acute mental health concerns or risks to himself or others. Between November 2017 and August 2019 there was no further contact with mental health services. Adult B remained under the care of his GP and medication advice was provided to his GP from mental health services. Adult B had a range of prescribed medication for physical health and mental health, which included anti-anxiety and antipsychotic medication for schizophrenia.
6.13 Agencies involved
The agencies involved with Adult B were an adult social worker (Torbay), GP, Accommodation provider and supported living staff, mental health services, Independent Care Act and Health Complaint Advocate, Enabling service for one-to-one hours, police, and the ambulance service.
6.14 Forensic history / Police involvement
Adult B did not have any convictions or cautions. Police had contact with Adult B in 2004, which led to a physical and emotional abuse disclosure in an Achieving Best Evidence (ABE) interview. In 2009, Adult B was reported missing, and police were involved in a child protection strategy meeting because Adult B set up a camera in his bedroom at the residential home that overlooked the playground of a school. In Aug 2019, Adult B made disclosures to supported living staff at the time his mental health had deteriorated, that he wanted to harm himself and had sexual thoughts about children, this was reported to police. In June 2020, Adult B disclosed he had downloaded indecent images of children (IIOC), this was investigated but none were found. A Vulnerability identification Screening Tool (ViST) was completed, outlining the deterioration in mental health, and child protection concern and sent to Torbay and South Devon Foundation Trust single point of contact (SPOC). Adult B was then referred into the Multi Agency Public Protection Arrangements (MAPPA)[12] process. In July 2020 police considered B under the Potentially Dangerous Person Process (PDP)[13]. Adult B did not meet the threshold for MAPPA or the PDP process. The telephone number of a helpline was also given to B called ‘STOP IT NOW’ for people concerned about sexualised thoughts about children.
[9] The Care and Support (Eligibility Criteria) Regulations 2014. An adult’s needs meet the eligibility criteria if—(a) the adult’s needs arise from or are related to a physical or mental impairment or illness; (b) as a result of the adult’s needs the adult is unable to achieve two or more of the outcomes specified in paragraph (2); and (c) as a consequence there is, or is likely to be, a significant impact on the adult’s well-being.
[10] Devon Partnership NHS Trust (DPT) is a mental health trust providing mental health services (adult and older persons) and learning disability services in Devon (excluding Plymouth). The Trust works in partnership with other organisations including Devon County Council, Torbay Unitary Authority and third sector organisations. DPT also works in partnership with other organisations to provide Children and Adolescence Mental Health services (CAMHs)
[11] the process of differentiating between two or more conditions which share similar signs or symptoms.
[12] MAPPA Criteria – Every MAPPA offender must be identified in one of the three categories. Category 1 – Registered sexual offenders as specified under Sexual Offences Act 2003, Part 2: Notification and Orders (on the Sexual Offenders’ Register); Category 2 – Violent offenders and other sexual offenders who are not required to register: An offender convicted (or found not guilty by reason of insanity or to be unfit to stand trial and to have done the act charged) of murder or an offence specified under Schedule 15 of the Criminal Justice Act 2003 (CJA 2003) Schedule 15 Criminal Justice Act 2003 who received a sentence of 12 months or more or a hospital order; An offender barred from working with children under the DBS Vetting and Barring Scheme (or subject to a Disqualification Order for an offence listed under Schedule 4 of the Criminal Justice and Court Services Act 2000, which preceded this Scheme). Category 3 – Other dangerous offenders: a person who has been cautioned, reprimanded, warned or convicted of an offence which indicates that he or she is capable of causing serious harm and which requires multi-agency management at Level 2 or).
[13] College of policing( Feb 2017 – updated 2020) Although not defined in statute, a PDP is a person who is not currently managed under one of the three Multi-Agency Public Protection Arrangements (MAPPA) but reasonable grounds exist for believing that there is a risk of them committing an offence or offences that will cause serious harm. a person charged with domestic abuse offences on a number of occasions against different partners but never convicted of offences that would make them a MAPPA-eligible offender, an individual who is continually investigated for allegations of child sexual abuse but is never charged or never receives a civil order, but whom agencies still believe poses a serious risk of sexual harm to children, a person suspected, but not convicted, of terrorism or extremism-related activity, where a community psychiatric nurse (CPN) or other mental health worker shares information with the police that a patient with mental ill health has disclosed fantasies about committing serious violent offences. The patient is not cooperating with the current treatment plan, and the informant believes serious violent behaviour is imminent. a person who has committed offences abroad that, had they been committed here, would result in the offender being managed under MAPPA.
7. Thematic explanation, analysis and findings
7.1 The key events identified were used to evaluate and explain professional practice and capture learning. Relevant research and wider evidence of effective clinical and professional practice, learning from local Devon male suicides, and the National Confidential Inquiry into suicide and safety in Mental Health (NCISH) (2019,2021,2022) formed part of the analysis. The analysis looks at how direct practice unfolded the way it did for each person and considers the factors that influenced practice within organisations and interagency working.
7.2 The care and support of the three men was provided at a difficult time for all agencies. The pandemic impacted on how care and support was experienced and how services in mental health
were prioritised and delivered. Observations made in the analysis are drawn from information provided to the SAR and interviews. Practitioners can only ‘know what is knowable at the time’. Understanding what happened and why requires understanding of the local rationality of professional practice,[14] and “hindsight bias”[15] should be avoided. The LR, upon drawing all the information together, has a window on events from all agency perspectives, allowing reflection on practice and systems through a ‘different lens’.
7.3 Whilst the three men had different individual circumstances, there were a number of parallel themes. These are summarised as trauma, mental health condition (more than one), poor and relapsing mental health, expressed thoughts of suicide, depression, anxiety, history of self-harm and suicide attempt, and excess alcohol use. Other connecting themes was that of communication difficulties at times of high levels of distress, difficulty or declining to engage with treatment or services, and two men had supported living placements where there was a breakdown of this placement with escalating risk. Two men described how they would end their lives and made an earlier attempt shortly before death.
7.4 The following themes listed in the table below were identified in this SAR. Some also feature in other local SARs and in the Local Government Analysis of Safeguarding Adults Reviews (April 2017 – March 2019). These are system problems likely to be repeated in other cases.
| Themes in this SAR |
Themes in Southwest SAR report |
| Direct Care | |
| Mental Capacity – Decisional and executive capacity | ✔ |
| Risk assessment male risk factors | ✔ |
| Carers assessment | ✔ |
| Communication family, referral outcomes | ✔ |
| Mental health relapse | ✔ also found in recent local SAR |
| Engagement with care and support | ✔ |
| Recording – accuracy of information | ✔ |
| Alcohol | ✔ Attention to MH |
| Clinical presentation / Diagnosis incl. Mental health and learning disability | ✔ Attention to MH |
| Self-neglect | ✔ |
| Dual diagnosis | ✔ |
| Interagency Working | |
| Access to mental health history | ✔ |
| Information sharing internally and interagency | ✔ Records sharing |
| People in need not meeting service criteria | ✔ and found in recent local SAR |
| Safeguarding – raising concerns process | ✔ |
| Collation of personal history | ✔ |
| Escalation protocol | ✔ |
| Multi-agency working and cooperation | X |
| Breakdown in package of care with escalating risk | ✔ |
| Interagency working and cooperation | X |
| Over reliance on emergency services for mental health crisis | X |
| Organisational Features | |
| MH resources face-to-face assessment, reliance on emergency services | ✔ Resources/workloads |
| Access to mental health inpatient beds | X |
| Services experienced as not meeting need. Client and staff. | ✔ Personalisation |
| Wait times in ED | X |
| Knowledge – trauma informed | ✔ |
| Access to specialist advise | ✔ |
| Local Authority boundaries | X |
| Gaps in services | ✔ |
| Other | |
| Impact of pandemic on people and services | N/A |
[14] The Local Rationality Principle encourages an understanding of why a decision, action, or error that seems irrational in hindsight, was actually the most rational choice at the time. It helps to understand the context of contributory factors influencing services and provides understanding of events, skills, and constraints.
[15] Hindsight bias is the tendency to ‘consistently exaggerate what could have been anticipated in foresight’ (Fischhoff, 1975) and is well reproduced research finding. Outcome bias is an element of this whereby we judge decisions or actions that are followed by a negative outcome more harshly than if the same decisions or actions had ended either neutrally or well. Blaming bad outcomes on simple causes such as human error can literally seems to make sense because knowledge of the outcome changes our perspective so fundamentally (Woods et al., 2010).
8. Direct work with individuals with care and support needs
8.1 How well the men’s health and social care needs met is explored using the wider terms of reference. The pandemic ran from early March 2020 – February 2022 when all restrictions were lifted, and England returned to the ‘living with covid’ strategy. Mental health need was the main factor in the circumstances of how events evolved. Adult C died at the time the rule of six was implemented for indoor and outdoor gatherings in September 2020, followed by Adult N who died just after the second national lockdown in early November 2020. Adult B was the third man to die, shortly after the third national lockdown in January 2021. Mental health deterioration for two of the men started late 2019, and in mid-2020 for another. This SAR found that during the pandemic the men’s health and social care needs were partially met, with difficulty in engagement and access to mental health services. The was a feature in all cases.
8.2 Generally there are a range of services available and working with men who have complex mental health. Mental health and the Adult Social Care (ASC) act as a conduit for commissioning other services to meet individual needs from a variety of providers and charities. Funding comes from care act funding, some via health funding, (within a reasonable budget), and some are personally funded by individuals with sufficient financial resources. Additional packages of care to provide one-to-one support are available as an add on to core hours in supported living. As a broad description, services work flexibly as multiagency partners. Inter-agency collaboration fluidity and mutual support is reliant upon mental health services having resource and capacity to step up their involvement at times when the support packages need help to continue. Alongside this there is access to out of hours services for mental health support and psychological services for anxiety and depression. There is also access to drop-in centres and help lines, provided by partner agencies and the voluntary sector.
8.3 Health Care is provided via primary care GP services who deliver a range of physical health care and specific health checks, i.e., learning disability annual health check, diabetes monitoring. There are referrals and emergency admission to the general hospital and other health services. Mental health care is provided by the local statutory services Devon Partnership NHS Trust (DPT). This includes adult and older persons and learning disability services in Devon (excluding Plymouth). DPT works in partnership with other organisations including the local authorities, third sector organisations and in partnership to provide Children and Adolescence Mental Health Services (CAMHS). There are dedicated specialist mental health teams and services for first contact and assessment, with provision of a range of out of hours services. Adult Social Care is provided by Devon County Council and Torbay and South Devon NHS Care Trust. These services are for adults for whom activities of daily living can be difficult (because of illness, older age, or a disability) helping them to live as independently as possible. Housing options include affordable housing via home choice, private rental, home ownership, shared ownership/leasehold, shared lives schemes, extra care housing/ supported living, care homes and short-term crisis and respite options.
8.4 Considering the question of what is working well from resources available, taking account of the pandemic, the following observation was made. All services involved engaged well with the role they were commissioned to provide. Adult social care, mental health care, supported living, other commissioned services, GPs, and general health care services all worked well individually. The mental health FRS, assessment service, psychological therapies, drop-in centres, and support services work well in circumstances where the person is motivated and able to use self-direction and reassurance, at times of increased anxiety. Agencies and other services collaborated effectively with mental health services until concerns about deteriorating mental health and a breakdown in the supported living package of care were referred to mental health for assessment, help, and specialist advice. At this point the function of the commissioned services faltered, and Adult C and B risk became unmanageable due to levels of distress and deteriorating mental health.
8.5 In this SAR there were barriers identified by agencies and services. One significant barrier in the care of Adult B, was the inability to access flexible mental health and learning disability services, to gain a comprehensive and specialist assessment. SAR information described that accessing mental health services was difficult. Other comments included that services were criteria focused, with no flexibility for people who do not fit neatly into criteria. Obstacles illustrated included reduced attendance at supported living premises, difficulty accessing face to face assessments and difficulty gaining guidance at times of crisis. Another observation made was that these difficulties were not isolated to the pandemic, but at other times pre pandemic and since. Agencies and services also identified difficulties with information sharing from mental health about history and risk. It was reported that information was difficult to obtain for two of the men, and that this was an ongoing problem experienced with other individuals.
8.6 Services described as missing by those involved included specialist consultation, mental health expertise, and guidance, with access to relevant training and support for partner agencies when working with people who had complex mental health needs. When exploring what service would have filled the ‘gap’ experienced, the service described was one that would attend housing, provide help, advice and support even where individuals were not open to mental health services. The service outlined to the LR best fitted a form of consultation and outreach service. Although there was access to the FRS, this was not experienced as helpful by Adult C and Adult B, or by the services involved. Another service missing was one that worked flexibly with people who had both mental health and learning disability needs. Another gap in services described by mental health managers related to the criteria for accessing talking therapies. To gain the maximum improvement requires Individuals to have a level of motivation. This service does not engage with people who had suicide or self-harm attempts within six weeks as this was considered too high risk, and the service requires alcohol use to be controlled. It was described to the LR that there was a gap between the self-access crisis services and talking therapies where people fell through the gap.
8.7 Conversely, in response to the gaps identified and the services described as missing, mental health services identified a disparity in their funding, and commissioning arrangements affecting what and how services can be delivered.
8.8 Generally from material provided to the SAR, and observations made by those involved, when thinking about improvements in support, the main comment was the difficulty experienced in accessing mental health services. The views expressed included improvement was needed for more face-to-face contact, and more flexibility to be responsive to people using services. GPs identified the need for more consistent and easily accessible ways of discussing mental health needs for people supported by primary care. Escalation protocols for fast and timely discussion about distressed individuals who fall outside of service criteria were needed. This was defined as a protocol with the power to ensure that services and agencies work together to respond promptly during times of crisis, even when there is disagreement among agencies, and when the circumstances do not align with the current safeguarding adult escalation policy.
8.9 Adult social care’s IMR for Adult B, identified improvements were needed in consultation and education, for communicating with someone when they are in a state of distress. Adult B was making genuine pleas for help, and the response to such pleas was considered more important than establishing whether the person fitted service criteria. Comments were made, that if services such as mental health cannot offer case management, can they offer robust consultation for adult social workers and care staff in terms of risk management and care planning?
8.10 Services were addressing the needs of this group of men via the usual organisation operational policies and protocols. Services work in partnership with statutory agencies commissioning other support services as required and using sign posting to voluntary, community, and social enterprise VCSE[16] sector services where this is indicated. The aim was to keep the person as independent as possible and for them to remain in their own homes. Adjustments were made to service delivery during the pandemic as per government advice. Devon mental health services brought forward plans for the Access and First response service (FRS) to have a service 24/7. This service was introduced in March 2020 as phone-only, with referral onto other services for face-to-face assessment. There was a triage function and outcomes ranged from telephone support or onwards referral to another mental health team, psychological therapies, or other relevant support options.
8.11 As a rule, services engaged with people who present with distress and active thoughts of suicide as was indicated in line with their agency purpose, policy, and procedures. Assessment of need and risk was undertaken at the time of contact, with referral onto other services as indicated For each man, practitioners involved responded to distress and active thoughts about suicide as the person presented face to face or via the telephone. Practitioners used the tools and structures of their services, policies and procedures, both single and multi-agency, for example referring into adult safeguarding with concerns about risk to self and children. On a day-to-day basis practitioners worked in partnership with the men using their care plans, risk assessments, and knowledge of the person. Staff also used therapeutic relationships, de-escalation techniques at times of distressed and disturbed behaviours. When needed practitioners and care staff requested and implemented advice, shared concerns with other agencies, sought supervision, and asked for help.
8.12 Examples of good practice for engagement with the men are seen in the interactions from supported living, the adult social worker (Torbay), and mental health services, who were kind and compassionate in response to distress and behaviours in the most difficult circumstances. Supported living staff were innovative in dealing with a situation involving risk to others using distraction and offer of activities. The Crisis Resolution Home Treatment Team (CRHTT) in May 2020 were able to engage well with Adult B which resulted in an improvement in mood, reduction of anxiety and agitation. Care staff and GPs followed care plans and tried to distract Adult C and B using techniques identified by the men themselves and mental health service advice. GPs in their contact with Adult C, B and N also used the distraction and relaxation and encouraged the men to use these techniques.
8.13 There was good practice from all agencies in contact with the men in their ability to engage with very distressed individuals to gather the appropriate information from them at a difficult time. There was kind and compassionate contact and engagement with Adult N and Adult C shown by ambulance staff on their attendance. Ambulance, police, GP and supported living were able to engage the men in discussion about thoughts and plans to end their lives. ED staff were able to engage with Adult B and facilitate his assessment by liaison psychiatry at a time of massive demand on services. The adult social worker (Torbay) was practical at times of distress and when B got a new phone, care staff were asked to input the telephone numbers for out of hours support. In March 2020 the adult social worker was advised by care staff that Adult B was verbalising thoughts about jumping from the building. In response to this the adult social worker undertook a face-to-face visit with B, although at the time he was not an active client on the case list, however the knowledge and relationship the adult social worker had with Adult B was the conduit to the follow up. The adult social worker used processes to engage Adult B to enable him to have some control and influence in events, and in the review of his package of care, this was good practice. The adult social worker liaised with the GP, and explored ways to help B communicate how he was feeling, although communication aids were refused. Supported living were responsive and flexible, attempting to meet the needs of these men and respond to their increasing levels of distress with kindness and structured support.
8.14 Largely the engagement approach was person centred and flexible, taking account of the presentation and situation at the time. There are a range of examples of good practice in person centred and flexible approaches. The ambulance crew used their own assessment of Adult C, who they assessed was not safe to leave at the accommodation when mental health staff advised he would be safe to leave as he was waiting for a support visit. The ambulance service responded to calls, made contact, face-to-face and telephone, attended the home address, spoke with the men, carried out physical health assessment, mental capacity assessment and conveyed them to hospital when this was indicated. In the circumstances of Adult N, information provided, suggests the contact with ambulance staff was more conducive to Adult N talking about the situation. When contacted, the police responded to each man as per their processes relevant to the presenting issue. The police had a number of face-to-face encounters with Adult C and Adult B, which were person centred, proactive, responsive and respectful, and support was provided to care staff. On the day Adult C died, an officer stayed at the home address due to the agitated behaviour, allowing the staff on duty to make calls to mental health services and GP for crisis advice. This was good practice and evidence of interagency cooperation.
8.15 There was good practice from mental health staff working in FRS, who attempted to engage with the men when they called the service expressing distress. Responding to someone in these circumstances and making an assessment during such a telephone call, is often difficult. When the call was ended by the men, staff contacted relevant other agencies to hand over information. Mental health services were also person centred in providing contact details for out of hours support for Adult C, B and N. The supported living staff were aware of individual need, their difficulties and provided support, prompting, enabling, made referrals as required, and facilitated reviews with key agencies.
8.16 GPs involved were flexible, and person centred. Primary care systems often led to appointments with the GP available on the day of appointment rather than a dedicated GP. For these men, the GP who had the most contact with them, responded to calls from staff and Adult C, B and N in the main. This was good practice. In Adult B circumstances the GP in telephone consultations did manage to engage with B despite communication limitations. This is evidenced by B initiating contact with the GP when in an agitated state. Other primary care health needs and risk were also responded to flexibly i.e., when the GP Phlebotomist service raised concerns about B’s intimidating behaviour at the surgery, a male health care assistant attended B’s accommodation to take bloods. This was good practice. Good practice was seen in response to Adult B’s physical health needs, managed via the GP and general hospital. Care included ongoing monitoring and responding to acute problems and when admitted to hospital learning disability nurses provided support, this was good practice and a person-centred approach. Another example of good practice in person centred, and flexible care, was the input from the advocate. It is noted that the commissioned advocacy service did not hold an NHS complaints contract for the Torbay locality, however the advocate continued to help with because of their knowledge and relationship built up with Adult B.
8.17 Although there were many examples of good practice, the three men had mixed experiences of person centred and flexible approaches to their care needs. Agencies responses to the pandemic required prioritisation of resources and some changes in the way in which services were delivered, taking account of Government Covid 19 direction and advice, although Adult social care (Torbay) describe maintaining interventions throughout the pandemic to meet legal duties. The need to prioritise resources specifically impacted on mental health support.
8.18 Adult B experienced inflexibility to his care needs because of his perceived cogitative difficulties. Internal referrals for Adult B were made by adult mental health to the learning disability service, and these bounced back as an inappropriate referral, at a time of acute distress and deteriorating mental health. In the IMRs and in discussion with relevant managers and staff, views were expressed that mental health services were less person centred with Adult B. Views were expressed by those who knew him, that he needed more time to take on board what was being said and time to respond. The LR considered outcomes from mental health was in part, as a result of contact with B where he was unable to respond quickly to questions, and on the requirement to prioritise responses to all the referrals made to the service. Individually there was limited flexibility from mental health services at the time of contact with the men, although the introduction of FRS and its ethos was flexible, and person centred. This was a crisis line for people to use when they felt they were in crisis and did not require a professional referral.
8.19 The LR analysed the key events identified in the chronologies see Appendix 2,3, and 4 with footnotes. The men’s mental health needs were the primary factor in their circumstances, as evidenced by the key events and their unfolding. The men’s perception of their needs differed to that of mental health professionals. This is not unusual, although the LR comments the levels of distress for each man, especially for Adult C and Adult B were severe.
8.20 There were various contributory factors to the difficulties in mental health care which impacted on how care was delivered, and how the men engaged (or not). With the advantage of knowing the outcome of events and looking at agency information together, the following influenced events and actions. These are seen throughout this report as the emerging themes and are clustered into categories. Individual patient factors – engagement in treatment and refusal of services, excess alcohol use, communication, mental health relapse, mental capacity – decisional and executive, and self-neglect. Operational factors – mental health resource, the impact of the pandemic on people and services, the demand on mental health services, the need to prioritise urgency, limited ability for face-to-face assessment, service criteria, gaps in services, and breakdown in the support package during crisis with escalating risk. Risk assessment – accuracy of information, information sharing, collation of history, different agency perspectives, perceived protective factors, verbal assurances of no plans to self-harm and key information unknown to mental health services. Multi-agency working – knowledge and skills of staff, and interagency cooperation.
8.21 Adult C wanted hospital admission to ‘fix his body and brain’, although it is not clear if his focus was on psychiatry or physical health care. His care and intervention were experienced through the lens of dependant personality disorder[17]. Admission to hospital was considered as not indicated during times of crisis as he was perceived as lacking in confidence to take personal responsibility. At times when C was in a state of heightened anxiety and refusing to take anti-depressant medication, he was unable to be reassured. Mental health services have a commitment to work in partnership with people with personality disorder in structured ways, sadly Adult C was not able to do this during his crisis. Upon reflection services appeared distracted and overly reassured by the package of care in supported living and one-to-one enabling services. Adult C’s needs from his perspective were not met.
8.22 The mental health IMR for Adult C includes his diagnosis as dependant personality disorder, an anxiety, acute stress reaction, and moderate depressive disorder. The consultant psychiatrist’s witness statement for the coroner’s inquest documents further information, that of a diagnosis of a recurrent treatment resistant depressive illness with atypical features and complex presentation with dependant personality traits, fear of coping alone, and a pattern of expressing suicidal thinking as a way of communicating his distress. It was unknown if the personality traits were lifelong or caused or exacerbated by his long experience of illness. The care coordinator included in information to the coroner that Adult C experienced severe depression with psychotic symptoms, suicidal thoughts, anxiety, and an inability to cope. The rationale for the primary focus on dependant personality disorder in C’s care is not clear. Without more information, understanding the events in the context of the level of distress, mental health crisis, C’s views about medication, and whether these were delusional in their intensity, is difficult.
8.23 There was treatment for alcohol detoxification in Nov 2019, and further concerns that Adult C was using alcohol in the months before his death. The SAR was not provided with information about exploration of the later alcohol use. The care coordinator reported he spoke about poor memory, that he was agitated and believed his brain was damaged. In January and February 2020, he stated he thought he had dementia. Adult C made multiple daily statements that his brain and body was not working properly. In a past hospital admission (2017) with a similar presentation, Adult C was admitted to the older persons mental health ward. It is not known whether dementia was a clinical consideration in this admission. Concerns about his brain not working was a longstanding concern. The brain scan in 2017, repeated in May 2020 did not provide reassurance. The 2020 scan results showed some evidence of a previous stroke and “a degree of cerebral atrophy greater than expected for age, but no significant change from a previous scan”. The LR comments on information provided to the inquest, that by the summer of 2019, Adult C couldn’t deal with everyday life. Adult C is described as making the same statements about medication, every time new medication was prescribed, he stopped taking it, he was restless, pacing, unable to sleep at night, he lost interest in activities he once enjoyed, followed his partner everywhere, and that he depended on her too much. The GP in the summer of 2019 referred C into mental health service with low mood and memory problems. The NHS website includes information about common changes to behaviour with onset of dementia. The LR is not making a diagnosis, but comments on the similarities which make interesting reflection of the reported behaviours, acknowledging dementia was a concern for him.
- loss of memory and thinking skills.
- repeating the same question or activity over and over again.
- restlessness, pacing, wandering, and fidgeting.
- night-time waking and sleep disturbance.
- following a partner or spouse around everywhere.
- loss of self-confidence, which may show as apathy or disinterest in their usual activities.
8.24 Adult B was consistent with thoughts about suicide and mental health deterioration since August 2019. Adult B is noted to be a risk to children. There was concern expressed about his behaviour around local schools, this was identified in agency reflection as a distraction for mental health services and it impacted on assessment of need. There is an assumption made that B’s distress and anxiety is because of the police investigation into IIOC on his computer. The chronology outlines the deterioration in mental health and distress started some time before this. Adult B’s limited communication and inability to engage in psychological therapies, due to learning disability, is the reason given as to why there was no alternative service to offer. Adult B also had a diagnosis of schizophrenia and he described hearing voices. Thought blocking, and poverty of thought are negative symptoms of schizophrenia, this may have been a factor in his inability to communicate. Staff describe he would start a conversation, there would be a long gap before he spoke, and he appeared to be listening to something. In February 2020, the GP made a referral into mental health services and an outpatient appointment for March 2020 with a consultant psychiatrist for a medication review was offered. This appointment was then cancelled due to the pandemic and the need to concentrate on urgent referrals. This was a missed opportunity to consider the full picture of his mental health. In May 2020 Adult B had an episode of care with the CRHTT. The team record a longstanding mood disorder with possible psychotic overlay at times, with OCD component, recent deterioration in mood with exacerbation of OCD, intrusive thoughts and increasing distress. When discharged nineteen days later the team note there is significant improvement in mood and reduction in anxiety and agitation, with no psychotic or delusional symptoms elicited at discharge. Another potential influence to deteriorating mental health was Adult B’s diabetes. It was known that B was not monitoring his blood sugar accurately a few months before his death.[18] A review of Adult B’s physical health was advised in September 2020 in the MHAT assessment, which ended before conclusion, due to distress. It is unknown whether his diabetes was reviewed, and if there was any link to his deteriorating mental health considered.
8.25 As the CRHTT intervention was successful in improvement of Adult B’s mental health, it is not understood why with a significant mental health diagnosis, that mental health could not offer a service. At the same time as Adult B’s cognitive deficits were highlighted as the reason that mental health are unable to provide a service, Adult B is then signposted to online and community resources with the NSPCC and the Lucy Faithful Foundation (LFF). These resources are for people who have concerning thoughts about harming children. Both resources require Adult B to cognitively engage in therapy, which appears incongruous, given Bs cognitive deficits are a barrier to accessing mental health services.
8.26 The focus of care and intervention for Adult N was the excess alcohol use and his mental health was viewed through this lens. He told his mother that he would have liked an assessment by mental health services rather than being sent home, although while at ED, he declined assessment. Equally local drug and alcohol services did not show curiosity to the number of referrals and attendances at ED. The level of depression was not explored further after discharge. Adult N told the ambulance and ED staff, he was not taking medication for depression, but told the GP he was. Adult N disclosed more information to ambulance staff, wanting to die, wanting to sleep and not wake up, relationship breakup, being lonely, and no access to the internet. There were concerns about self-neglect. Adult N verbally reassures services he knows how to get help but did not or was not able to follow this through. This raises the question of whether this was related to reduced motivation and mental capacity, due to the depth of his depression and, or alcohol use? His mother described at inquest that since the pandemic there was a decline in his mental health, and he was consuming large amounts of cider a day. There was no detail to the levels of alcohol consumed in the assessments made in ED,
8.27 The collation of personal and mental health history is a theme in this SAR. History, and personal information about Adult N, C and B appears unknown to mental health services. The mental health IMR notes that Adult Ns first contact with services was in 2017. Earlier contact from 1993 for severe depression with psychotic features and four episodes of treatment for depression and anxiety in later years from 2008 to 2014, is not referred to. There was limited information about his social history, the breakdown of his marriage and no detail about his employment history, and why he has not worked for a significant time. Key information was unavailable to mental health staff. It cannot be known this information would have changed the assessment and intervention, but this is significant to risk assessment context. In Adult C’s care, important background history prior to his first mental health contact was not known. Family recall that his mental health significantly deteriorated after the death of a parent, describing he was never the same man again. Details of this information generate questions about trauma as a child and information might indicate other siblings were affected. Relatives of Adult C’s raised questions about information discussed at the inquest that was not included in the IMRs, that of the consideration of autism and a request for supported living to undertake an online autism assessment. There was no further information about this available.
8.28 Another example of unknown information is the assessment of Adult B in 2008, which concluded that he was not eligible for an ongoing learning disability (LD) service due to the low level of impairment. The mental health IMR makes no reference to this and may account for why internal referrals were made to LD services. This is potentially a systems problem related to history taking and, or access to past mental health records. In June 2020 Adult B is described in a letter from mental health services to the GP as having a borderline learning disability, with possible diagnosis of autism. There was no other information about this, and autism did not feature in the information provided to supported living, nor was the adult social worker aware of this information.
8.29 Contributing factors to events were the different views and perspectives of the men, supported living staff, GP and mental health services. Events were all seen through different knowledge, and viewpoints. Irrespective of the approach taken by services, the men did not feel listened to, with events experienced as mental health not responding to their high levels of distress. This was also the experience of supported living staff and the GP. With the assistance of being able to see all the information together, the LR reflects that mental health relapse factors were not assessed as relapse, but more as behaviours stemming from the diagnosis. An example of this can be seen when reflecting on information, levels of concern and distress expressed by Adult C in August 2020. Adult C is highly distressed and agitated, unable to focus on aspects of daily living and disruptive to other residents. Adult C made multiple calls to services and ambulance asking for help. Responses are observed to be delayed and incongruent, he appeared low and flat in mood, care staff describe episodes of disassociation, he is non concordant with treatment and his views about medication may be delusional. At this point FRS determined that referral to and assessment by CRHTT was not indicated as Adult C had a good package of care in place. Supported living staff expressed dissatisfaction with this outcome and requested additional social care hours for one-to-one support.
8.30 Police and ambulance services are the first point of call when the men were in crisis. Emergency services have most of the face-to-face interactions along with the supported living staff. The men’s mental health had deteriorated to the degree that, with the aid of seeing all the agency information, the men required a more in-depth assessment and that their care and support packages via commissioned services had broken down and staff felt unable to manage the deterioration.
8.31 In mid-January 2021(14th) the adult social worker was trying to get the right support for Adult B at the multi-disciplinary meeting. The adult social worker requested expertise from learning disability and mental health services, stressing the importance of needing advice of where he can get the right support. The LD service emailed their apologies and suggested increasing one-to-one time as a distraction to B’s intrusive thoughts. This was already in place and did not have effect in reducing distress and turmoil. The request for help and expertise was not forth coming. Other services and professionals state they were left holding the risk with complex individuals. Agencies commented staff had rightly escalated concerns to mental health, but the response they got, after being redirected to several points in mental health, was not always the most helpful.
8.32 In Adult Ns contact with ambulance staff, he made a disclosure about how he is feeling, he was isolated and lonely, sharing detail he has no access to the internet. The ambulance crew appear to have an opportunity to build some trust for disclosures to be made. This is perhaps because at the point of contact, N is distressed and responding to their enquiries and concern. The ambulance crew recorded details of what was happening from his perspective. This information was not in ED and liaison psychiatry IMR, and it is unknown if this detail was passed on in full.
8.33 Practitioners at ED had five encounters with Adult N over seventeen days. How long he was in the ED is unknown as details of time of arrival and time seen were not provided. On the first attendance (15/08/2020) it appears that Adult N was in the ED for around six hours. Details about his presentation while he was waiting are unknown. In contrast to what was shared with the ambulance staff, he appears to be less communicative and was minimising his actions, giving opposite information. On 20 and 22nd August 2020, Adult N states to liaison psychiatry he does not know why he took an overdose, denying wanting to end his life, that he had no plans and just wanted to get home as he was concerned about his mother. The discharge from ED included a support plan also referred to as ‘safety netting’, and included a range of contact numbers and services for him to call when he needed support.
8.34 Liaison Psychiatry have a difficult task, they make assessments for people presenting with self-harm in a difficult setting, often with limited information except that gained from the individual who may or may not give a full account. Adult N may have lost the ‘moment’ where he felt able to disclose and talk about how he was really feeling. Likely cause was the lengthy wait times in ED to be seen. The LR did not have the opportunity to discuss with liaison psychiatry and therefore hypothesizes that the lengthy wait (due to demand on services and therefore unavoidable), was not conducive to a man in distress. The opportunity to disclose in detail what was happening, how he was feeling, and any active thoughts of suicide was reduced and impacted by the passage of time. It is perceived likely, all he wanted to do was get home, possibly needing to consume alcohol to prevent withdrawal, and therefore more likely to tell staff what he thought they wanted to hear, that he was not planning to harm himself and to minimise his actions to provide them with reassurance. This is not unusual and a difficult phenomenon to predict and manage at an ED presentation. This issue will be repeated in other cases of self-harm.[19] This is not a criticism of ED and liaison psychiatry staff, simply an observation about very busy services and the difficulties of making assessments in this setting. The coroner inquest for Adult N saw liaison psychiatry give evidence that the service was under immense demand at the time, with patients waiting outside in ambulances for hours, as there were no beds and no room in the ED department. This finding is system related and is one that occurred in all three and likely to repeat in other cases.
8.35 Adult B communicated his distress that he was ‘going insane’, that he wanted help, he could no longer tolerate the intrusive thoughts. In late April 2020 adult B stated he would kill himself and described how he would do this, by stabbing himself or jumping off the building. Adult B acted on these plans in September 2020, he tried to stab himself with a screwdriver or cutlery, causing bruising and scratching. In early January 2023, two weeks before his death, he was seen going to the top floor. When asked, he said he was going to jump off the building, he returned to his flat with persuasion from staff who remained to provide support with his distress. Adult B shared this information with FRS but ended the call when staff tried to use grounding techniques with him. Supported living referred the concerns to the adult social worker, GP and mental health services and escalated concerns through their managerial structure.
8.36 Adult social care reflected that B needed specialist support to help deal with his feelings of despair. With a dual diagnosis of learning disability/difficulty and mental health the adult social worker considered this was a barrier to him receiving the specialist support required. He did not meet the criteria for either the Mental Health Team or LD specialist services and he slipped through the cracks. Specialist teams’ criteria’s can be very rigid. Adult social care staff recorded they would like to see this changed so that the person is seen as a whole rather than by their diagnosis. Agency IMR reflections noted, had Adult B received a psychological assessment, that this may have helped him process what was happening to him and why. This could have also been invaluable in supporting those working with B on a day-to-day basis, and in some ways, they could have been providing informal therapeutic input, or at least provided him with a greater level of understanding. The IMR concludes the adult social worker and the supported living staff were just firefighting as best as they could because they did not have specialist skills, or the advice required. This was despite the pragmatic steps taken by the adult social worker to refer and communicate information in a multidisciplinary meeting in an attempt to get the right support. ASC IMR also reflected on communication with a person when they are in a state of distress. He was clearly asking for help, yet his mental health assessments were brief due to his lack of engagement and distress. There was a belief based on the experience of working with B that there was a need to build a relationship where he could be open and honest and that he needed time to process questions. It was considered possible, had staff with a relationship with him been present at the assessments, whether the team could have drawn different conclusions. In other comments re Adult B, staff questioned whether the mental health team should be thinking outside of the box regarding how they provide therapy to someone that struggles to engage rather than dismiss this as an option. It was acknowledged that this could be a lengthy piece of work but questioned that this was time well spent rather than the loss of someone’s life. To underpin the points raised in IMRs, a learning disability manager confirmed there was an expectation that people with learning disabilities and mental health will access mainstream mental health services where the learning disability need is considered as not reaching the threshold of a specialist service. It was acknowledged that in reality because people like Adult B needed significantly more time to help them to engage in assessments and talking therapies, it had become more difficult for them to receive a service.
8.37 In November 2020, Adult B with support from the advocate made a complaint to mental health services. This was a specific complaint about lack of assistance offered, and failure to provide a mental health service. As a result of the conclusion that Adult B did not meet criteria for the provision of services, his needs were not met. The desired outcome was that services be provided to him to mitigate his risk of harm to himself and to others. The response to this complaint and outcome of was not provided to the SAR. This was relevant information and could have helped provide further understanding of the rationale behind decision making by mental health services.
8.38 The LR considered the “No Wrong Door”, vision for mental health, autism, and learning disability services in 2032[20], published Dec 2022. This paper explains why services for mental health, autism, and learning disabilities need to reform. Ten essential components of the vision are listed in the study as: 1. Prevention, 2. Early intervention, 3. Access to quality, compassionate care, 4. Seeing the bigger picture, 5. Whole-person care, 6. Equality focus, 7. Co-production, 8. Boosting autonomy, human rights and community support, 9. Thriving, diverse and effective workforce, 10. Measuring the outcomes that matter. This vision highlights some of the issues raised about Adult B’s inability to access services and falling between the gaps.
8.39 The receptiveness of the men and their ability to put into action the supportive directive prompts was a contributory factor to the limitations of the advice and guidance from FRS. This was likely due to levels of anxiety and distress. A telephone assessment of this would be difficult, particularly with Adult C, and there are clinical records with similar behaviours. These note contacting services were a form of self-rescue rather than relapsing mental health. For Adult C the engagement with health services, and their advice was challenging to hear. Adult C verbalised that he did not feel listened to, and in his note to his family found at the site of his death, he wrote that “.. services and others were pitted against him”. On one occasion he stated to mental health services “I came here for help” “You cannot keep sending me away” and “I want hospital admission”. On another occasion he called the 111 service twice in a day (12/04/2020) and ambulance staff were sent to make an assessment. Adult C was described as fearful and distressed, that he wanted to be taken to the general hospital for a brain scan, stating he wanted “proper treatment and not to be sent home”. He was not taking prescribed medication because of his fixed belief that these were harming him. This was key treatment in the course of his illness and one that Adult C could not come to terms with.
8.40 Care and support planning requires the individual to be involved and the plan should meet the needs and achieve the outcomes of what the person wants. In law the local authority and health must genuinely involve the person in the planning of their care and support – described as person centred and person led. The planning process should be built around the person’s wishes, feelings, needs, values, and aspirations. Adult C and Adult B, specifically asked mental health services for help, expressed their distress, an inability to manage anxiety, intrusive thoughts and feeling unsafe. Their requests for help to mental health were not responded to as they had wanted, as these were assessed within the parameters of the diagnosis, engendering self-help, support, and independence with the protective factors of a supportive care package.
8.41 The Mental Capacity Act 2005 provides the legal framework for acting and making decisions on behalf of individuals who lack mental capacity. The Act applies whether the decisions are life-changing events or everyday matters. [21] There are systems, policies and processes for agencies and providers to undertake assessment.
8.42 The ambulance crew assessed mental capacity for all three men with regards to conveyance to hospital. There were other points in the care where mental capacity was considered. Adult C’s mental capacity was considered in relation to prescribed medication when in respite supported living (Dec 2019). As part of a Mental Health Act[22] Assessment undertaken, consideration was given to whether C was delusional in his views about medication, and if his mental capacity to make decisions about this was impaired. There was further assessment of mental capacity about increasing care provision in June 2020, although this assessment was not completed as he was unable to engage, the decision was made to increase the care package in his best interests.
8.43 Adult B’s mental capacity was considered in a mental health assessment when he was unable or unwilling to discuss his intrusive thoughts further. It was observed his answers appeared to be learnt rather than spontaneous and it was difficult to assess if he had mental capacity to answer the questions. In July 2020 Adult B’s mental capacity to instruct an advocate as a means of involving B in his care was recorded. In September 2020 it was believed adult B did not have mental capacity re medication, he was declining to allow supported living staff to help him with this. There were other concerns about self-neglect in Dec 2020, where he was deemed not to have mental capacity due to his deteriorating mental health.
8.44 There was consideration of Adult Ns mental capacity on his third attendance at ED, staff record that he understands his risk of self-discharge and verbalised he understood the risk. The lack of clarity in the documentation of a more formalised mental capacity assessment is noted in the learning from ED, that mental capacity could have been documented more clearly. This is a much-repeated theme in other SARs.
8.45 The LR reflects that decisional and executive functioning is not referred to in the MCA nor the code of practice, but it is part of the assessment for some decisions and has been highlighted in many SARs about self-neglect. These are the contextual terms describing challenges of assessing mental capacity, when the person can verbalise the decision, but not put it into action. This is described as when they can ‘talk the talk’ (decisional capacity) but cannot ‘walk the walk’ (executive capacity), that is they cannot carry out the actions for the decision, “because of an impairment of, or a disturbance in the functioning of, the mind or brain. Decisions in mental capacity assessments can be decisional (just in the moment) and decisional and performative in their nature (i.e., application of information also takes place outside of the discussion)[23]. This is relevant consideration for Adult C, B and N.
8.46 It is possible the amount of alcohol use and or the level of N’s depression meant he was unable to take forward referrals made to alcohol services. The LR comments that the ability to follow guidance was likely impaired for all three men. Although the men did contact services, they were unable to put into practice what was advised. In Adult Ns situation, establishing outcomes of the referrals to alcohol services was an opportunity to further assess mental capacity, decisional and executive functioning. Professional curiosity after the multiple ED attendances to follow up on referral outcomes may help to address refusal of services. The question arises, as services are currently commissioned, which service would undertake such follow up from an ED attendance if the person did not meet the threshold for mental health services?
8.47 When considering mental capacity in this SAR the LR notes that social care documentation suggests more confidence about the assessment and the recording of the decision.
8.48 Adult C had a care coordinator and was open to mental health services. At the time of placement in supported living the care plan was three weekly contacts with the care coordinator. Prior to this, contact was described as weekly. Adult B and Adult N were not open to mental health services and there was no case management for either. Adult N main point of contact was via the GP, noting that Adult N was not open and honest with the GP. Adult B was referred into adult social care at times of crisis. The responses and action were undertaken by the adult social worker who knew him well, this was good practice. Although Adult B was not open to the adult social workers case load formally, the work was allocated, and a relationship was maintained due to his vulnerability. The same adult social worker was the point of contact for the supported living staff, this appeared to be an informal arrangement, and gave out her mobile number as a way of providing some additional support to the staff. This was a good example of agencies working together. The adult social worker went the extra mile in response to the level of concern, to provide support with a complex, difficult situation.
8.49 Risk assessment for these men were undertaken by individual agencies at various points as events unfolded. Risk assessment for suicide is not an ‘exact science’. Clinical messages from the National Confidential Inquiry into suicide and safety in mental health (NCISH) 2020, 2021, 2022, includes that risk assessment tools should not be seen as a way of predicting future suicidal behaviour. That risk is not a number and risk assessment not a checklist, it needs to be simple, accessible and should be considered part of a wider assessment process. The emphasis of risk assessment should be on 1. Building relationships, 2. gathering good quality information on current situation, 3. Past history and 4. social factors to inform a collaborative approach to management. The collation of history, and unknown information are features in this review. Adult C’s daughter shared with the LR that her father told her he did not expect to live beyond 60 years, and he died three days before his 60th birthday. After death when C’s room was cleared, papers were found of notes about the ‘pros and cons’ of living or dying. This was not known prior to death. At Adult C’s last MDT meeting there was no direct enquiry about thoughts of suicide.
8.50 Research into suicide[24] highlights in clinical risk there are established risk factors for suicide, which include: previous self-harm, alcohol or drug misuse, multiple mental health diagnoses, diagnosis of personality disorder and increased risk of impulsivity, living alone, and gender. Males between ages 50-54 were found to have the highest suicide rate. Warning signs of suicide are described[25] as talking about wanting to die, great guilt or shame, being a burden to others. Common feelings experienced among patients who die by suicide are described as feeling empty, hopeless, trapped, or having no reason to live, extremely sad, more anxious, agitated, or full of rage, and unbearable emotional or physical pain. All three men experienced and verbalised similar thoughts and feelings to these warning signs. The men also fall within the male risk factors, age, and circumstances. The latter was not referred to in any risk information provided.
8.51 Responding to loss of contact with services is an important prevention measure. Assessment of risk should include significant dates and anniversaries which may then form part of safety planning. Risk assessment now includes asking about internet and social media[26] use by the person. Self-harm or risky behaviour may also be considered as a potential rehearsal for eventual suicide. For Adult B, Adult C and Adult N, this was not considered at the time, repeat behaviours with the potential for death followed by seeking help was seen as a positive protective factor. Seen in the context of rehearsing to end their lives, this was in fact a far greater risk than was previously understood. Rehearsal of suicide[27] is referenced in the mental health IMR for Adult C and B, and states that literature on suicide describes ‘rehearsing’ as the deadliest of preparatory behaviours. Local learning in this area is described as gaining greater understanding and to challenge a number of misconceptions relating to people who express suicidal thinking and behaviours.
8.52 Suicide prevention during COVID-19 advice centred around clinicians being aware of the need to maintain support for patients under the care of mental health services, particularly for patients who are anxious, isolated or have experienced disruption to care. The lockdown during the pandemic prevented Adult B and Adult C from using their normal coping strategies and their distress increased.
8.53 The introduction of FRS service during the pandemic for anyone who was experiencing mental health difficulties or crisis as defined by them, was pioneering. There was no time to test the service out to iron out various teething problems, this was done as the service was delivered. FRS was a means to get support, guidance and where needed signposting to other services, and agencies. In other examples of good practice in managing risk, in Adult C care, concern was expressed about his safety to drive and support staff were responsive and innovative in managing this risk. On one occasion staff prevented C from using his vehicle by blocking it in with another car as a short-term solution, while advice was sought. Distraction was then used with Adult C, until he was diverted to another activity and lost interest in wanting to drive. Potential risk to self and others in allowing him to drive was recognised in ‘real time’ and a risk reduction strategy applied. Good specific advice was provided by the social worker assigned to mental health services and the GP about how to report to the DVLA and how fitness to drive would be assessed. Supported living were respectful and responsive to this risk and took timely and appropriate action.
8.54 The risk assessment used by FRS was the UK Mental Health Triage scale, see Appendix 5. With limited information from mental health about risk assessment it was difficult to comment in any depth. Superficially the LR considered information from agencies and interviews, descriptions of behaviours and how agency records reflected the situation. Within the triage scale, the circumstances and risk (in the LRs opinion), fell into the definition between code B, C, and D and potentially E (E was a non-urgent mental health response), although the latter requires that other services can manage the person until the mental health assessment. It is acknowledged the LR was not present at the time of assessment. Looking at information, the ‘typical presentation’ described in the triage scale for Adult C and B indicated a face-to-face assessment in a short time scale (four hours, twenty-four hours, and seventy-two hours). Looking at events for both men, the assessment of the call was triaged as code F or G. This is an outcome of the referral not requiring face-to-face response and resulted in actions such as provision of advice, support, and, or referral to other providers. The LRs view of how contact was assessed is supported by the grading recorded on letters to the GP dated early January 2021, where Adult Bs call to FRS was graded at G, advice only.
8.55 In Adult C and Adult B circumstances, partner agencies and services involved conveyed to mental health services they were struggling to support the men. In March 2020 Adult B disclosed to support staff thoughts about jumping off the balcony. In Adult B’s situation, agencies and services are described by the GP as having reached the ceiling of their intervention and needed more specialist input from mental health. One IMR stated “Neither the social worker nor supported living staff could have been expected to have the specialist knowledge required to judge what was going on for B, nor did they have the necessary suicide prevention skills”. The GP made a referral to mental health services in early January 2021, after supported living staff contacted the GP to report Adult B had attempted to access the top floor. The GP included in the letter that “supported living staff could not provide a 24-hour suicide watch, noting that it was difficult for trained clinicians to confidently know that this was manipulative behaviour, and the GP would not expect support workers to have to make that decision”.
8.56 One consistent risk factor for each man was ongoing suicidal thoughts, some with identified methods, plans and evidence of acting on these i.e., going to the cliffs, self-harm, and overdoses. Adult B made threats to kill himself which included the method, and he attempted this four days before his death. In contrast, mental health records note after contact with the men, there were no thoughts, or some thoughts, but no plans. Information about Adult B becoming paranoid was not explored further, or details were not provided to the SAR. The significance of the men’s earlier actions and risk are mitigated by supported living and the understanding the men were seeking help before harming themselves. The GP referral in January 2021 is recorded in the response letter as ‘declined’. The rationale identifies supported living staff can manage by encouraging B to return to his flat and locking the doors. Protective factors are noted as supported accommodation and staff having locked the doors to the top floor as they are concerned B may attempt to end his life. It is unclear how the protective factor of supported accommodation was determined, given the concerns raised by the staff and the GP about inability to manage suicidal behaviour. The GP is informed the adult social worker has been asked to arrange a multi-disciplinary meeting to discuss the way forward. Advice and guidance are given to the GP about implementing the previous recommendations for medication in September 2020.
8.57 There are inaccuracies in mental health information that influenced risk assessment. One example of this was information in August 2020, Adult N’s risk to self is assessed as moderate as this was his first overdose, and he had sought help. This is not his first overdose and N gives information in ED that he took an overdose some years ago. No details of exploration of this were provided. Adult N is also noted by ED, after the fifth overdose in a short succession, that he had no plans, yet this was an admission for a repeated self-harm attempt. Looking at the information given by Adult N on each the overdoses, he is consistent when speaking with ambulance staff that he wants to die. Another example in Adult B’s care, the April 2020 risk assessment recorded the predisposing risk (what does not change) as learning disability but does not include the diagnosis of schizophrenia. Protective factors are recorded as access to mental health services and housing support. This was not accurate, as B cannot access the services he needs, and supported living were asking for help from mental health. Other inaccurate information is that of Adult B counting numbers. This is recorded by FRS as helping him distract himself. B had stated to support staff that he finds his inability to stop the compulsive counting of numbers and their hierarchy, known only to him, as an acute stressor increasing his distress. With the help of seeing all the information together, descriptions of events indicate mental health relapse was prominent in Adult B’s situation.
8.58 Clinical risk policies within Devon’s mental health services used the following scale[28] in April 2019 and this applied to all potential risks, including risks to self and others. Circumstances for Adult C and Adult B (in the LRs opinion) using these descriptors, are assessed as high risk at certain points of events.
- High risk: Individual who presents a risk of acting in a way – either planned or spontaneous – which is very likely to cause serious harm. Limited protective factors to mitigate or reduce that risk, requires active risk management, planned supervision and close monitoring, intensive treatment to decrease risk.
- Medium risk: Individual who is capable of acting in a way that could cause serious harm but there are sufficient protective factors to moderate that risk, mental capacity to engage with risk management strategies and may respond positively to treatment. This individual may become high risk in the absence of the protective factors.
- Low risk: Individual who may or may not have caused, attempted, or threatened serious harm in the past but a repeat of such behaviour is not thought likely between now and next risk assessment, engages well to risk management planning and responds to treatment.
8.59 There were a range of factors that influenced risk assessment and provided assurance for the three men. These are seen as previously understood self-protective behaviours, the support packages, alcohol service engagement, accessing out of hours, verbal assurance that the men would not harm themselves and engaging in treatment. With the benefit of knowing what happened, these factors did not provide the desired reduction of distress. Knowledge of Adult C included behaviours that could be seen as manipulative. One example of this was a call to services stating he was having suicidal thoughts, yet he was seen at the time of making the call, in a que waiting to purchase ice-cream. There was a perception when in respite care that Adult C called services with statements about wanting to die to escalate service responses. FRS assessed the presenting risk with the men at each contact. Enquiries were made about thoughts and plans to self-harm. Reassurance was gained by the men not verbalising any plan. The LR comments that the notion of assurance from the person to keep themselves safe is unreliable, as in (now outdated and no longer used) suicide prevention contract, with an agreement not to die by suicide. There is also the argument of coercion or pressure placed on the person to provide reassurance, the person is often keen to tell the other what they think they want to hear, not wanting to worry them, hence this is unreliable. Mental health service assessment information for these men is reliant upon the protective factors of supported living, and additional one-to-one hours. This was a distraction because supported living staff, the adult social worker and GP were asking for help due to their concerns of escalating distress and risk, that they were unable to manage.
8.60 Consideration of risk in Adult B’s circumstances, encompassed known information, and this was interpreted as B’s usual way of responding and he was not presenting differently. FRS Risk assessment noted that B was unable to say why the crisis had emerged, he was coherent, orientated in time and place and did not indicate any strange ideas or belief. When Adult B said he was having a panic attack, normal breathing was heard, and when attempting to explore options, he ended the call. These factors raised doubt that Adult B was in crisis and what he was describing was ‘normal’ for him. Taking account of all the information together, there are alternative interpretations; that Adult B was unable to voice his thoughts due to thought blocking, a symptom of schizophrenia, and, or his level of depression reduced his communication. It is known that the number counting was not a distraction but a symptom that increased his distress, these may have been auditory hallucinations[29] (voices). Adult B told staff the OCD behaviours were linked to the number counting, and the numbers were linked to thoughts and voices he heard. Adult B had a list for the meanings of the numbers, seven was about sexual harm to children and eight was harm to staff. Adult B declined to tell staff what the other numbers meant, he said he did not want to upset or hurt anyone.
8.61 When the GP referred Adult B into mental health services in January 2021 asking for help, FRS assessed the information, and referred this to the MHAT. The team did not think anything had changed but acknowledged B was more distressed. It is unclear why this is interpreted as unchanged as the increased distress is recognised. FRS made a call to Adult B as support and summarised the information in a letter format for the GP. Information provided in the letter was already known to the GP and did not provide a solution. The planned multi-agency meeting is noted for discussion and a date is given when mental health staff could attend, although this meeting is not immediate. The meeting did not take place immediately despite the heightened concerns about risk. The timing of this meeting was reliant upon mental health staff attendance and at this time due to demands on services staff have limited availability.
8.62 In Adult N’s risk assessment, the following were considered as protective factors: his mother, no active plans to end his life, “self-rescue”, reporting a desire to reduce his alcohol intake, being insightful, and that he was now “willing to work with services”. It was not unreasonable for the risk assessment to conclude that these were protective factors, although there was no consistency demonstrating Adult N was able to engage in services.
8.63 Communication was a theme within this SAR, influencing risk assessment, how crisis and the breakdown of the care package was communicated and understood. Terminology used to describe events hold different agency perspectives and minimised risk. The concern that Adult B walked out in front of a moving car was reported as a concern for road safety, yet before the pandemic Adult B regularly walked to his voluntary work, crossing multiple roads safely. The actual description in the enabling service IMR, stated that he walked into the road with moving cars and on occasions would lay down. The LR questions was this an attempt to end his life? Other terminology used by agencies, exactly what was said and how it was interpreted remains unclear. Examples of this are supported living staff expressing extreme concern for Adult C, and that Adult B was not expressing strange beliefs, when he was stating he would make an attempt on his life and how he would do this. The terminology used appears to be received and understood differently from mental health service perspective.
8.64 There was a range of learning identified in IMRs related to risk for example, ED should refer everybody who has taken an overdose to the Liaison Psychiatry team, as directed by NICE best practice guidelines. This did not happen for Adult N on two subsequent attendances for self-harm. Additionally, when a person is not referred on to secondary assessment services, individualised safety planning with people should be completed. Since the deaths, mental health services responded quickly to learning from the National Confidential Inquiry into Suicide, making changes to the clinical risk assessment and management policy. Information was circulated to staff as updates to the clinical risk policy. A rewrite of this policy was completed in 2022, moving away from checklists and ‘low, medium and high’ ratings, with emphasis on personalised approach and safety planning; to include competency assessment. There has also been a change in training around suicide, incorporating local learning, starting in early 2023. Learning from events of Adult C, B and N was circulated to staff. This included personalised risk, that self-rescue should not always be considered a protective risk factor, self-harm or risky behaviour may also be considered as a potential rehearsal for eventual suicide, and the use of direct enquiry into suicidal thoughts at each contact. These changes are good practice and evidence of a learning organisation.
8.65 Taking account of the length of time since the deaths of the three men some three years before this SAR was completed, relevant information from national statistics for England and Wales and key learning from suicides are included to provide balance.
- Since 2010, men aged 45 to 64 years have had the highest age-specific suicide rates. Male rates for all age groups were higher in 2021 than in 2020, except for those aged 75 years and over where the rate remained unchanged.
- 2019 – There were 4,303 male suicides. The age range of 45-49 was the highest age specific suicide rate. The most common method of suicide was hanging.
- 2020 – There were 3,925 male suicides. There was a decrease in male suicides at start of pandemic and delays in registration due to pandemic. Males and females aged 45 to 49 years had the highest age-specific suicide rate.
- 2021 -There were 4,129 male suicides. The rates of suicide were consistent with the pre-coronavirus (COVID-19) pandemic rates in 2019 and 2018. Men aged 50 to 54 years had the highest age-specific suicide rate. The most common method of suicide for both males and females was hanging, strangulation and suffocation (all grouped together). The second most common method was poisoning.
8.66 The national confidential inquiry into suicide covering 2009 – 2019 included key findings of interest, with parallels found in this SAR:
- The majority of patients who died had a history of self-harm (64%) and there were high proportions of those with alcohol (47%) and drug (37%) misuse, and comorbidity, i.e., more than one mental health diagnosis (53%).
- Nearly half (48%) lived alone. In 13%, the contact with mental health services was a one-off contact. In 9%, patients were known to have died on or near an anniversary or significant date.
- Experiences of the pandemic, for example anxiety, isolation, and disruption to care, may have contributed to some suicides by mental health patients.
8.67 Parallels seen here, are the methods used, that of self-poisoning, followed by hanging, and jumping from a height, histories of self-harm, excess alcohol and more than one mental health diagnosis. One man died two days before a significant anniversary and each man experienced isolation during the pandemic, disruption to their care and usual coping mechanisms.
8.68 To look briefly at local factors, basic data was requested for the years 2019 – 2021, to consider data for the year before the pandemic, during, and after. The following table includes coroners’ verdicts of suicide/taken own life. A basic analysis of data shows the number of deaths appear to follow the national trends, in that there was no evidence of increase in suicides during the pandemic locally. Male suicides were higher than females in all three years. The data does not include narrative verdicts and there may be other suicides yet to be confirmed by the coroner. Of the three men who died, two deaths are included in these figures. Mental health services do not currently keep data on narrative verdicts and did not have capacity to extract this information for this SAR.
| Local Mental Health Data on Suicides/Taken Own Life | |||
|---|---|---|---|
| 2019 | 2020 | 2021 | |
| Total deaths | 29 | 16 | 15 |
| Male | 18 | 9 | 8 |
| Female | 10 | 7 | 6 |
| Blank | 1 | 1 | |
8.69 In general discussion with the Mental Health Deputy Director of Nursing for Patient Safety, the emerging themes were discussed. The following areas of ongoing improvement work were highlighted as relevant to this SAR and are included to illustrate the action and learning already undertaken.
- Quality of risk assessments
- Safety planning and risk formulation
- Family involvement
- Stronger together – families and carers
- Training
- Mental capacity – assessing and application, recording and need for training.
- Alcohol services – staff now make referrals on behalf of patients rather than advise to self-refer.
- Closer working with the voluntary and charity sector
- Working with personality disorder
The LR also was made aware that recently mental health services led on development of a crisis advice flow chart to help other partners access the right support.
8.70 In addition to the improvement work in mental health services, there is a range of ongoing suicide prevention work in line with national policy,[30] which provides the framework for local suicide prevention strategies and action plans. The Devon wide Suicide Prevention Statement and action plan adopts the national strategy framework which outlines two principal objectives: reduce the suicide rate in the general population and provide better support for those bereaved or affected by suicide. There are seven priority areas:
1. Reduce the risk of suicide in key high-risk groups
2. Tailor approaches to improve mental health in specific groups
3. Reduce access to the means of suicide
4. Provide better information and support to those bereaved or affected by suicide
5. Support the media in delivering sensitive approaches to suicide and suicidal behaviour
6. Support research, data collection and monitoring
7. Reducing rates of self-harm as a key indicator of suicide risk
8.71 The local 2022-23 action plan includes priorities for short-term action which are relevant to this SAR: reducing risk in men, preventing, and responding to self-harm with a range of services for adults and young people in crisis, and psychosocial assessment for self-harm patients, treatment of depression in primary care, adequate bed numbers, tackling high frequency locations including working with local media to prevent imitative suicides, and reducing social isolation.
8.72 To meet these priorities, Devon and Torbay Council continue to work closely with mental health. The mental health safe from suicide team have a ten-point plan, which includes more relevant actions: low staff turnover, outreach teams, personalised risk management, guidance on depression, and 24 hr crisis teams.
8.73 In the delivery of the care and support there was limited or no liaison with family members. It is not known how background information and mental health history was collated for each person. The lack of family involvement in collation of personal history and mental health history is a factor repeated in other people’s mental health care and is a missed opportunity to gather all the relevant information. For Adult B there was no close family contact, and no one involved in his life. Adult N lived with his mother and when assessed in the ED there was no contact with his mother. This was learning noted in the ED IMR. There was no information of whether Adult N had ever received or been offered a carers assessment. The lack of carer assessment is a theme in other SARs and one that may be repeated in future cases.
8.74 There was good practice in case supervision found in Adult C and Adult B case. Case supervision was sought by the Torbay adult social worker who had most contact with Adult B from the line manager and the senior practitioner for social work. Supervision was requested by the adult social worker at times of concerns for adult B’s welfare, suicide risk and inability to access mental health services. Supervision was also sought in January 2021, when extreme concern was expressed for B’s welfare and risk of suicide. Case Supervision was also sought by the advocate allocated to B in July 2020.
8.75 The description of FRS includes access to senior clinicians for advice and supervision for tele workers to discuss cases and contacts with the service. It is not known if any supervision was offered in relation to contact with Adult C, B or N. Support was offered to supported living for Adult C and B after their deaths by mental health service managers, this was good practice. One feature of a supportive organisation is where supervision is provided enabling reflection on the situation, a recognition of challenges working with very complex distressed people and case oversight. Information to the SAR provided does not allow further comment.
8.76 Safeguarding is the responsibility of every agency and organisation, “safeguarding is everybody’s business”. Adult and Child safeguarding is led by the local authority. It is a statutory requirement for all agencies and services to engage in partnership work and prioritise safeguarding. Structures and processes for this are formally embedded in organisational policies and procedures that ‘dove tail’ into the overarching multi-agency policies. The work is to protect those who are at risk of harm from others or themselves. This SAR was triggered by three deaths where distress, threats of suicide and access to mental health support was difficult during the pandemic. One referral included “that relevant agencies failed to work together robustly enough to prevent death occurring, and that he had ongoing mental health problems and staff have made numerous referrals for him to the mental health services, but he has not received any help”.
8.77 Consideration of safeguarding was seen in the care of Adult C, Adult B and Adult N. There was good safeguarding practice by supported living and police about B’s self-disclosure of images of children on his computer and other historic offences. Police took his concerns seriously and an investigation of material on his laptop was commenced. Adult B also disclosed other offences that he abused others as a teenager, these were also investigated. None of the victims wanted to come forward. Relevant safeguarding information was given to these individuals to access support. Disclosures of physical and sexual Abuse of B by his parents and a teacher at his school were taken seriously and enquires made, but could not be taken forward, the parents were deceased, and the teacher could not be identified. The police also considered public protection processes in relation to Adult Bs thoughts about harming children.
8.78 Safeguarding was implemented using the relevant safeguarding policy and processes. In 2017, good practice in child protection was seen when Adult C’s stepson’s welfare was considered during deteriorating mental health, and children’s services were alerted to the situation. In June 2020 Police made referrals to Torbay adult safeguarding single point of contact for Adult B, with concerns about deteriorating mental health, risk to self and potential risk to children. The triage of the safeguarding referral records an outcome of no adult safeguarding concerns. The second safeguarding referral early January 2021 recorded concern about B’s attempt and statement that he was going to the upper floor to jump off the building. This referral was again assessed as not meeting s42 criteria threshold for a safeguarding enquiry. This was to be addressed via risk management and a referral was made into adult social care. This was an appropriate response, although the issue of inability to access mental health services does not feature in the triage decision. Potentially there was an adult safeguarding concern. At the time of this referral Adult B was unable to access mental health services in the last six months despite deteriorating mental health, with referrals made by GP, adult social worker, and supported living. In theory this could have been considered under category of discrimination, the inability to access mental health services, or organisational abuse, or neglect, that B’s mental health needs were not addressed. Although this was not considered under safeguarding, a complaint was made about B’s inability to access the mental health support he needed with help from an advocate.
8.79 In another safeguarding referral the concern was interpreted differently by the local authority due to the language used. On 4th September 2020 (day of Adult C death) the ambulance crew made a safeguarding referral for Adult C about self-neglect and a frequent caller. This is recorded as a referral for welfare support on September 7th by adult social care and immediately sent on to the CMHT as he had an identified mental health worker. The process for the ambulance service to make a safeguarding referral requires the type of need to be identified in the email heading, i.e., a referral for welfare (adult social care response) or safeguarding. In previous SAR learning, inconsistencies in the title and content of the email referral from ambulance staff were highlighted as impacting on safeguarding responses. These inconsistencies appear yet to be resolved. A safeguarding referral was also made by ED for Adult N’s mother due to concern about her carers self-harm using her medication, and questions about his ability to undertake caring duties, this was good practice. Outcomes to these enquires were not recorded in the information to the SAR.
8.80 During agencies contact with mental health services, in the circumstances of Adult C and Adult B the safeguarding categories of discrimination, neglect and acts of omission or organisational abuse were not considered[31]. While this may sound controversial – the nub of events shortly before death is best described as; the telephone support was not experienced as reducing acute distress and their mental health continued to deteriorate. Concerns were voiced by all agencies including police and GPs, that mental health deterioration could not be managed within the care package, risk was escalating, and services were asking for help. The dictionary definition of neglect is ‘lack of care’. The safeguarding adult escalation policy[32] was not in place until October 2021, and the staff involved were not thinking ‘safeguarding’ as a route to emphasise their concerns and challenge decisions about access to mental health services. Was this a missed opportunity for rapid escalation of concerns within the context of the pandemic and service prioritisation? Discussing these concerns using safeguarding may have provided more focus on the seriousness of escalating events, and the adverse impact of service prioritisation. Safeguarding may have triggered discussion of this issue at a senior managerial level.
8.81 The mental health IMR acknowledged the legislation and policy guidelines in place to ensure all organisations respond to the legal obligations to meet individual communication needs, and the Equality Act. [33] The mental health IMR referenced these policies and commented that “…when decisions were made, mental health staff had collected all the information available to enable them to come to the correct clinical decisions. When B was not offered a service because mental health services were unable to meet his needs, staff remained open to discussions with all the services involved and a multi-agency meeting was held on 8th Sept 2020, and another was planned for 22nd January 2021.” The theme of communication and how this is interpreted by agencies is a critical feature of this. In the LRs opinion, the standards and principals of these policies were not implemented, there was no adjustments made and the meeting in Sept 2020 did not provide any solutions. The Equality Act 2010 is law that prohibits discrimination against people with protected characteristics, including disability. The act defines a disability as a mental or physical impairment that has a substantial and long-term negative effect on ability to carry out day to day activities. Communication difficulties may be considered a disability. The law requires that information and communication is accessible to everyone, and that no one is disadvantaged because of communication difficulties. According to the Social Care Institute for Excellence (SCIE), substandard service provision relating to a protected characteristic is a form of discriminatory abuse, including denying basic rights i.e. to healthcare, education, employment, relating to a protected characteristic.
8.82 There were other examples of where safeguarding processes potentially could have been considered. Self-neglect was a safeguarding category present in this SAR for all three men[34]. Concerns were raised with the ambulance service and passed onto ED about Adult Ns self-neglect, not eating properly, weight loss, excess alcohol, repeated overdose, and declining alcohol services. Adult C is reported to be self-neglecting, refusing treatment – medication, and there were concerns about his mental capacity to make decisions about this. Adult B is recorded a few months before death, as self-neglecting his personal appearance and daily tasks and declining to allow staff to support him with medication. It is acknowledged that the level of self-neglect described in the men’s situation, may not have been considered life threatening to warrant use of the safeguarding self-neglect process, when the focus was on accessing mental health support. Upon reflection of events, would a self-neglect referral have enabled further discussion with the men and services to review the situation?
8.83 Making Safeguarding Personal (MSP)[35] uses the DoH six principals for adult safeguarding. These principals were used in the care and support for Adult B, although there is less evidence of MSP in the care of Adult C and Adult N. Empowerment is seen in the work undertaken by the adult social worker involving Adult B in a range of opportunities for decision making in his care, protection is seen in police actions when adult B’s welfare was put before the disclosures of serious offences. Using the SAR process to identify learning, demonstrates the MSP principals of partnership, protection, prevention, and accountability in action.
8.84 There are a range of factors in the work environment that support good practice. Good knowledge of the people with care and support needs is essential to underpin person centred, needs led care and support. Essential to the latter is good record keeping, a comprehensive history, personalised risk assessment, responsive systems which have flexibility in access criteria, or consultation advice for crisis situations. Other factors are flexible interagency working providing care, information sharing, communication, cooperation, and increased interagency support at times of increasing distress and changes in mental health stability. Additionally adequate training is necessary to provide practitioners with the right skill set, good safeguarding knowledge and the ability to apply this to practice. When looking at factors that create unsafe conditions in which poor safeguarding practice is more likely, these same factors are relevant where these are limited or not available. Without repeating analysis in other sections, this SAR includes examples of the factors above which were both good and poor practice. The latter results in unsafe conditions. One area that warranted commenting on, was the quality of records and the information transcribed into the SAR documents. The IR observed multiple acronyms used in local services. The LR had to decipher what some of the acronyms meant, and in some cases was unable to identify meaning, and enquiries also failed to establish this, i.e. – Liaison advise that B be referred to DISCO and advice from community social care team, DISCO make a rapid re-referral to adult social care as B is SDHCT.
8.85 Trauma informed approaches have been developing since 2018. It is cited in policy, and adopted in practice more frequently now, as a means for reducing the negative impact of trauma experiences, to support better mental and physical health outcomes. Gov.UK notes the working definition will be kept under review, and the use of trauma-informed practice in different settings and sectors, continues to develop. [36] It is a service delivery approach weaving trauma knowledge and sensitivity into existing actions and models. Trauma-informed practice aims to increase practitioners’ awareness of how trauma can negatively impact on individuals and communities. It seeks to prepare practitioners to work in collaboration and partnership with people and empower them to make choices about their health and wellbeing. Trauma-informed practice acknowledges the need to see beyond an individual’s presenting behaviours and to ask, ‘What does this person need?’ rather than ‘What is wrong with this person?’. It seeks to address the barriers that people affected by trauma can experience when accessing health and care services. It is not about treating the trauma, that is recognised as the role of specialist services.
8.86 Being trauma-informed means assuming that people are more likely than not to have a history of traumatic experiences and that these experiences may impact on their ability to feel safe within or develop trusting relationships with services. Staff use the six principles of trauma-informed practice: safety, trust, choice, collaboration, empowerment, and cultural consideration. There are four stages: 1. Trauma aware: Staff understand trauma, its effects and survivor adaptations. 2. Trauma sensitive: The agency integrates some concepts of a trauma-informed approach into operational ethos, 3. Trauma responsive: Individuals and the agency recognise and respond to trauma, enabling changes in behaviour and strengthening resilience and protective factors. 4. Trauma-informed: The culture of the whole system, including all work practices and settings reflects a trauma-informed approach.
8.87 The NHS Mental Health Implementation Plan 2019/20 – 2023/24, sets out the NHS Long Term Plan (LTP). It covers Workforce, financial transparency, mental health equalities, acknowledges Adverse Childhood Experiences (ACE) and the link to trauma. Following the publication of this, the Community Mental Health Framework for Adults and Older Adults [37] was produced. This document sets out the vision and plan for a new community mental health model. The framework acknowledges the current model needs modernisation and refers to personalised and trauma-informed care among many much-needed areas of change.
8.88 Local mental health services have work underway in response to this plan. Their webpages about the implementation plan acknowledges issues raised in this SAR, that of difficulty accessing services, in particular the community mental health services for adults with severe mental health needs, long waiting lists, access to care coordinators, and access to CMHT due to service demand and pandemic restrictions. DPT acknowledges that people have fallen through the net, due to gaps in services. The implementation plan will tackle these issues to deliver more consistent, joined-up support for people that better meets their personal needs and the needs of their local community. DPT provided the LR with a brief outline of development work relevant to recommendations in this SAR. This included the development of trauma informed services. There is a training needs analysis, an outline plan for delivery of trauma informed practice training, a two-day course which is open to other agencies, delivered by Plymouth Trauma Informed Network.
8.89 From the review of events it is fair to say, during the care of these men, services were not trauma informed and had limited knowledge of this. However local mental health services and its commissioned IAPT providers do provide specialised evidence-based and evidence-informed trauma-specific interventions. The current gap in trauma awareness locally, was seeing beyond an individual’s presenting behaviours. These men did not have the opportunity to influence how their mental health needs were met, and services did not see their trauma. Barriers were experienced as distress for Adult C and Adult B, and in some respects for Adult N. This is not unique to Devon and is found in other mental health services, who will also be undertaking community mental health framework transformation work.
8.90 Agencies involved with the three men, had some awareness of individual trauma. Adult B’s disclosures of physical and sexual abuse were known, although it appeared that symptoms of trauma were not recognised in connection to his overall mental health presentation. Adult C experienced trauma from the distress caused by his mental health symptoms. His distress seen and responded to through the lens of dependant personality disorder. Earlier mental health interventions in response to similar symptomology and levels of distress, included formal and informal hospital admission. Looking back on this approach, Adult C mental health appears to have improved or stabilised upon admission followed by deterioration after discharge when he stopped medication. It is not known how access to inpatient beds during the pandemic may (or may not) have been an influencing factor. Health commissioners requested access to inpatient beds be included in the IMR report, but this information was not referenced. The LR does not know if this question was addressed. Mental health note discrepancies in funded mental health beds compared to other similar areas and populations. This is a systems issue, with a risk of repeating in other cases.
8.91 Whether agencies and services understood and recognised associated trauma impacting on Adult B’s mental health, is an interesting question. Events that unfolded suggest past trauma was not seen as a reason for his deterioration. Post traumatic stress disorder (PTSD) or Complex post-traumatic stress disorder (CPTSD) [38] and associated symptoms were not considered. Taking account of all the information together, including descriptions given by staff about B’s behaviour, his communication impairment, this offers argument, that he was experiencing symptoms of trauma. It is possible B’s focus on the intrusive thoughts of harming children were associated with re-living his own abuse, and, or the intrusive thoughts were voice hallucinations because of CPTSD or schizophrenia. Further consideration of B’s deterioration includes his inability to communicate and engage in treatment and support. A question arises, was B able to engage and follow the grounding and distraction techniques FRS staff tried to engage him with? This may not be related to mild learning disability or difficulties, but that talking about how he was feeling was triggering trauma and flashbacks of past abuse. This may be an explanation of why B terminated the call when FRS staff were attempting to help him and why B stated that talking did not help. The enabling service providing one to one support to distract B’s distress, reported shortly before death, that B did not talk much, but what he did say was about the horrible intrusive thoughts he had, and how he wanted these to stop.
8.92 In exploring B’s behaviour of laying down on the floor at the accommodation through the lens of trauma, the question arises, was B experiencing periods of disassociation?[39] Looking at this behaviour from CPTSD, was Adult B communicating his distress, and using his own technique for grounding himself in reality, by laying on the floor. Considering the Trauma Continuum,[40] from descriptions of behaviour and information known, it is likely Adult B would be assessed as experiencing type III trauma, multiple pervasive traumas from early age that continued over time and impacted on adult life. It is unknown whether B had an assessment for trauma. Staff recall B tried hard to tell the staff what was going on in his thoughts. He disclosed some of the images and thoughts he had, not only about children but also about the staff. The counting of numbers was associated with ‘bad things.” B would not disclose what all the numbers were, he said he feared what would happen if he told anyone.
8.93 In the circumstances of Adult N, the LR believes there was trauma as a result of grief stemming from the loss of his grandmother and loss of his marriage. The limited background and historical information provided, coupled with lack of access to past mental health history, prevents exploring Adult N’s trauma in any detail.
[16] The voluntary, community and social enterprise (VCSE) sector is an important partner for statutory health and social care agencies and plays a key role in improving health, well-being and care outcomes.
[17] April 2022: The latest revision of the International Classification of Diseases (ICD-11) no longer distinguishes the previous separate types of personality disorder, but defines it as a single condition, classified by severity.
[18] People living with type 1 or type 2 diabetes are at increased risk for depression, anxiety and eating disorders. Rates of depression across the lifespan are 2 times greater for people with diabetes than in the general population. www.ontrackwithdiaabetes.com – Individuals with diabetes may struggle with various symptoms caused by high or low blood sugar. High blood sugars tend to cause depressive feelings and mood swings, while low blood sugar may cause scattered thoughts while extreme lows can even cause hallucinations and delusional thinking.
[19] 2017 – RCN members have called on the college to lobby to ensure emergency departments (EDs) are no longer used as a designated place of safety for people experiencing a mental health crisis.
October 2021 BMC Health Services – Experiences of people seen in an acute hospital setting by a liaison mental health service: responses from an online survey: Patients should be seen more quickly in ED. Respondents felt that one hour should be the maximum somebody should wait if they have a significant mental health problem the time of writing, people in need or urgent mental healthcare will be seen within one hour of attending the ED by a member of the liaison team. Liaison mental health services in England are to be strengthened to meet this new target, with 70% of services meeting a core standard of staffing levels for size of hospital by 2023/24 and 100% coverage thereafter [22]. It remains to be seen if this new target for LMHS results in improved service user satisfaction. Conclusions Close attention must be given to evaluating and improving LMHS both from the organisational perspective (waiting times, clinical environment) and from the human side of the clinical interaction (staff attitudes and behaviour) as this experience can be inherently therapeutic while having implications on engagement with treatment and future psychiatric care.
[20] https://www.nhsconfed.org/publications/no-wrong-door December 2022 by the NHS Confederation in collaboration with the Centre for Mental Health.
[21] https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/921428/Mental-capacity-act-code-of-practice.pdf
[22] (MHA 1983, amended 2007)
[23] Dr Emma Cameron and James Codling Oct 2020. ‘decisional’ and ‘performative’ considerations. – This means the person has to understand, retain and use or weigh the relevant information, not only in the abstract assessment conversation, but also outside of this; applying information in practice at the time that they themselves need to make the decision. This could well be the case for social care practitioners when considering capacity in relation to: Care and support arrangements (especially in the context of self-neglect); Managing finances. Managing medication. Decisions about sexual relations.
[24] NCISH Annual Report 2022
[25] National Institute of Mental Health (NIMH)
[26] Royal College of Psychiatrists Self-harm and suicide in adults Final report of the Patient Safety Group July 2020
[27] Robert I. Simon, MD 2012 – Clinical Professor of Psychiatry, A suicide rehearsal is a behavioural enactment of a suicide method, usually as part of a suicide plan. A suicide rehearsal is a process that evolves over time into a plan. Patients who are intent on attempting suicide usually do not reveal their plans. However, behavioural rehearsals display specific clinical characteristics that speak louder than the guarded patient’s denials, revealing the patient’s suicide plan.
[28] This scale is slightly adapted from: Best Practice in Managing Clinical Risk (updated 2009) Department of Health
[29] Auditory hallucinations can range from mild distortions to voices when nobody is speaking. The voices may be quiet or loud, friendly or intimidating. Auditory hallucinations are the most common type that people with schizophrenia experience. Elizabeth Hartney, BSc, MSc, MA, PhD.
[30] Public Health England supported by National Suicide Prevention Alliance – Local Suicide Prevention Planning. A practice resource September 2020.
[31] Torbay and Devon Safeguarding Adult Procedures and Guidance Oct 2021. Organisational abuse – includes neglect and poor care practice…. It can be through neglect or poor professional practice as a result of the structure, policies, processes and practices within an organisation. Neglect and acts of omission – includes ignoring medical, emotional or physical care needs, failure to provide access to appropriate health, care and support or educational services and………. Neglect also includes a failure to intervene in situations that are dangerous to the person concerned or to others, particularly where the adult at risk lacks the mental capacity to assess risk for themselves. Discriminatory abuse includes harassment, slurs or similar treatment because of race, gender and gender identity, age, disability, sexual orientation or religion. Examples of discriminatory abuse may include denying access to communication aids, not allowing access to an interpreter, signer or lipreader. Harassment or deliberate exclusion on the grounds of a protected characteristic. Denying basic rights to healthcare, education, employment and criminal justice relating to a protected characteristic. Substandard service provision relating to a protected characteristic (SCIE 2015) – an example of substandard service provision is failing to provide someone with reasonable adjustments for their disability.
[32] Oct 2021 The aim of this protocol is to resolve professional disagreements relating to the safety of adults at risk, escalating any concerns that may arise, if issues are not viewed as being dealt with satisfactorily. Occasionally, situations arise when workers in one organisation feel that the decision made by a worker from another organisation regarding safeguarding an adult at risk is not appropriate. All workers should feel able to challenge decision-making. It is their right and responsibility, in order to promote the best multi-agency safeguarding practice. All workers have a professional duty to raise concerns about an individual at risk and all organisations should be mindful to give appropriate support to those raising a concern, as difference in status/experience may affect someone’s confidence in reporting.
[33] Accessible communication and information policy ‘communication principles and services available to staff, patients, their carers and relatives to ensure that no individual or group feels excluded from using services for any reason’. The need to: Meet individual needs: Ensuring steps are taken to provide the communication and/or information needs in the required accessible format, and Flag individual needs: Ensuring an electronic flag is visible on the electronic clinical record to highlight the individual has a communication and/or information need and ensures communication and/or information is given in the required format. Equality, Diversity, and Inclusion policy (G09- 2019) giving every individual the ability to achieve their potential through creation of a fair society. No person should be at a disadvantage or have poorer life chances because of their protected characteristics and individuality. Diversity is about the recognition and valuing difference in its broadest sense……. Inclusion at its simplest is the ‘state of being included’. It is about valuing all individuals, giving equal access and opportunity to all and removing discrimination and other barriers to involvement’.
[34]Torbay and Devon Safeguarding Adult Procedures and Guidance Oct 2021 Self-neglect This covers a wide range of behaviour neglecting to care for one’s personal hygiene, health or surroundings and includes behaviour such as hoarding. It should be noted that self-neglect may not always prompt a section 42 enquiry. An assessment should be made on a case-by-case basis. A decision on whether a response is required under safeguarding will depend on the adult’s ability to protect themselves by controlling their own behaviour. There may come a point when they are no longer able to do this, without external support.
[35] Making Safeguarding Personal (MSP) LGA with the Association of Directors of Adult Social Care (ADASS) briefing November 2019, MSP is not just about safeguarding practice but also about prevention, and strategic as well as operational safeguarding
[36] Gov.uk – working definition of trauma informed practice Nov 2022.
[37] September 2019 Prepared by: NHS England and NHS Improvement and the National Collaborating Central for Mental Health
[38] Mind.org.uk – Complex post-traumatic stress disorder (complex PTSD, sometimes abbreviated to PTSD or CPTSD) is a condition where you experience some symptoms of PTSD along with some additional symptoms, such as: difficulty controlling your emotions, feeling very angry or distrustful towards the world, constant feelings of emptiness or hopelessness, feeling as if you are permanently damaged or worthless, feeling as if you are completely different to other people, feeling like nobody can understand what happened to you, avoiding friendships and relationships, or finding them very difficult, often experiencing dissociative symptoms such as depersonalisation or derealisation, physical symptoms, such as headaches, dizziness, chest pains and stomach aches, regular suicidal feelings.
[39] Dissociation involves experiencing a disconnection and lack of continuity between thoughts, memories, surroundings, actions, and identity. People with dissociative disorders escape reality in ways that are involuntary and unhealthy and causes problems with functioning in everyday life. Dissociative disorders usually develop as a reaction to trauma and help keep difficult memories at bay. Symptoms – Times of stress can temporarily worsen symptoms, making them more obvious. Signs and symptoms depend on the type of dissociative disorders, but may include: Memory loss (amnesia) of certain time periods, events, people and personal information, A sense of being detached from yourself and emotions, A perception of the people and things around you as distorted and unreal, A blurred sense of identity, Significant stress or problems in your relationships, work or other important areas of your life, Inability to cope well with emotional or professional stress, Mental health problems, such as depression, anxiety, and suicidal thoughts and behaviours
[40] Betzy De Thierry 2019- The trauma continuum – type I single incident trauma, type II – multiple trauma and Type III trauma multiple pervasive traumas from early age. The continuum progresses according to the degree of trauma experienced. Type II trauma involves repetitive experiences that are terrifying, these can rarely be spoken about due to the shock, threats, loyalty issues, confusion or a dissociative response. Type III or complex trauma involves multiple different traumatic experiences that are serious and repeated, involved over many years. Complex trauma usually involves interpersonal violence, violation and or threat and is often longer in duration.
9. Inter-Professional and Interagency Collaboration
9.1 A range of services and agencies were involved in the care and support of the three men. Communication was internal and interagency including referrals and general communication, verbal, written, email, and telephone calls.
9.2 Concerns about inter-agency and inter-professional collaboration was the trigger for this SAR. Supported living staff and GPs did not feel supported by mental health services. Agencies commented that although the escalation pathways were generally well understood at operational level, when the operational pathways did not function as they should, support staff can be left dealing with very difficult and high-risk situations. Timely and appropriate escalation in such circumstances is critical. An example of what was not functioning (as perceived by other agencies) was the transfer of CMHT for Adult C. On the day of death, the supported living staff contacted the local CMHT with extreme concern for C and were advised he was in a three-month transition period from Exmouth, and that staff should call FRS. Staff then called the FRS and were put through to the CMHT in Exmouth, who advised to call his GP and request an emergency prescription for Diazepam to carry him through the weekend. Staff then called the GP surgery and arranged a call back. It is unclear how the extreme concern from C’s mental state was specifically communicated. Reflections by those involved are recorded in the IMRs, and one IMR records the “..events never truly being understood,……. but as agencies we must prevent this happening again…. Reflecting on the input from agencies involved……, I now question were we truly working in a multi-disciplinary way?” One example where agencies were not working together, was the concern that Adult B was a risk to children. The child protection concerns were not prioritised in any of the requests to mental health services for intervention for B. The LR again raises the question of how this was communicated to mental health, that there was a child protection concern and assessment was required?
9.3 In IMRs and interviews, agencies raised concern about the lack of information sharing from mental health services. Agencies spoke about the lack of history, contextual information about the risk of suicide. GPs noted delays in notification of contact with mental health services, treatment, and outcomes. Adult social care confirmed that information sharing from ED is a current concern. Adult social workers are not informed of outcomes unless they make numerous calls to ED. This is a systems issue and one that is repeated in other cases. Those speaking candidly gave examples; in Adult C circumstances, supported living staff were concerned that his mental health background, the high-risk manifestations of his illness, possibly due to non-compliance with medication between referral, assessment and placement was not shared. Managers noted whilst Adult C needs were within the criteria for admission, senior managers report they would have had pause for thought if they had known of his levels of acuity and risk behaviours at the time. Other examples were described in terms that conveyed extreme frustration around accessing mental health information. One agency commented “When we, (professionals) ask for information, we do so based on a genuine need to know more, and therefore request for information should not meet with the ‘data protection’ barrier”.
9.4 There was inter-agency working between police, ambulance, GPs, mental health – FRS, MHAT, adult social worker, mental health social worker and supported living. There were a range of good practice examples seen in multi-agency working, already noted in other sections. Another example is the support the police officer gave to supported living staff, after returning Adult C when he was a missing person, with concern for welfare. The officer stayed on at the home due to Adult C’s disturbed behaviour, while staff phoned for crisis advice, this was good practice and evidence of interagency cooperation. The FRS crisis service also included a dedicated professional’s line. All these services worked closely together, responding to how the men presented in crisis. Police and ambulance were the first call by the men themselves or by supported living. These were also the services staff were advised to call as a response to levels of agitation, distress and risk to other residents, children or staff. It needs acknowledging that some calls to emergency services were appropriate as the first line of response, for example, when Adult C was in a taxi on his way to the cliffs, and when Adult N took an overdose. When considering the overview of all the information, police and ambulance services provided a higher proportion of face-to-face contact during periods of high distress and mental health crisis. In the absence of mental health resource, was there an over reliance on emergency services to make face-to-face contact, and was there any alternative in the circumstances? This is a systems issue and one that is repeated locally and nationally.
9.5 Recent national attention in 2023, raised concern about the demands on police and ambulance services, in responding to mental health and self-harm incidents, at the cost of reducing the time available to respond to crime, and physical health emergency. The concern introduced new ways of working under the National Partnership Agreement. People experiencing mental health crisis will be attended to by medical professionals as the priority, rather than the police as default.[41] The new agreement is based on a model developed by Humberside Police called Right Care, Right Person, and the nationwide rollout coordinated by the National Police Chiefs’ Council (NPCC). Evaluation of the Humberside Police model found it saved the force 1,100 hours per month, and police still attend such incidents when needed. Evaluation included that the new agreement “rectifies what has clearly become a systemic problem” in policing. Other developments nationally include mental health ambulances designed to take specialist staff directly to patients and improvements to the NHS 111 and crisis phone lines. The mental health service IMR refers to the ‘Street Triage’, a mental health service working with police making sure that people who need mental health treatment receive it quickly, and appropriate information sharing takes place. This service is provided using the Approved Mental Health Professionals (AMHP) and covers Monday to Sunday, including weekends in core working hours and into the early hours. There was no detail provided if this service was involved with Adult C and Adult B, except that C called them regularly. In September 2023 as part of ongoing service development, this service now provides a 24/7 designated police direct telephone line through to FRS. Police are offered information sharing and section 136 consultation with a senior clinician, possible triage over the phone and face to face assessment when required.
9.6 There was good interagency working between ED, liaison psychiatry and mental health services. There was the facility created as a pandemic emergency response, to enable face to face assessments by mental health professionals at an alternative mental health hub when ED was at capacity. There was also good practice in internal agency working and interagency referrals. Referrals from ED were made to alcohol services for Adult N, with prompt response. It is not known if Adult N’s decision to decline assessment was communicated back to mental health services or the GP.
9.7 In Adult B’s circumstances there was limited flexible joint working between agencies. The adult social worker contacted the CMHT in December 2020, to seek support in attending a multi-agency meeting, and was advised that B was closed to their services and the GP would need to re-refer. There was no flexibility to bring mental health expertise quickly to a meeting. In December 2020 and January 2021, the GP contacted mental health and sent a referral asking for help. The referral was rejected and the meeting to discuss concerns is described as the way forward. The GP requested this be brought forward as this is two weeks away. This did not address the GP’s concerns and there was no plan for the interim, except to phone FRS if things deteriorated, which was the situation leading to the GP referral. When the date was set for the multi-agency meeting mental health staff have no capacity to attend quickly and a further sixteen days elapsed, and sadly adult B died three days before the meeting.
[41] Mental health professionals and police in specialist response cars https://www.itv.com/news/anglia/2023-01-14/how-nurses-and-police-are-joining-forces-to-help-people-in-crisis , mental health ambulances https://www.itv.com/news/calendar/2021-06-29/hull-trials-one-of-uks-first-mental-health-ambulances-following-spike-in-call-outs
10. Organisational features of agencies involved affecting how practitioners and teams worked
10.1 All services involved changed to some extent how they functioned in response to the pandemic and government advice. Services incorporated Gov directives, wearing face masks, limiting contact with others where possible and workers self-isolating. Mental health services made changes to service delivery at the time. Daily clinical advisory groups, that included directors and senior operational managers, were used to share risk decisions, and respond to fluctuating events. The introduction of FRS, working from home, use of video conference and telephone calls instead of face-to-face contact, and the community team’s re-prioritisation of caseloads to respond to urgent work, were all introduced to meet directives.
10.2 In mental health services at the start of the FRS service, responses were limited to telephone support. The service was staffed by redeployed clinicians and other staff. Staff needed to be trained quickly, needed supervision and support, and were required to pull together in a new role. The demand on the service was described at a level above that which the service was staffed to address. FRS implementation was brought forward by two months and set up to manage an anticipated 100 calls per day. The actual number of calls each day was well above this, described as between 150 to 200 calls each day. The service was not able to meet this demand, and the level of calls to FRS has not reduced since the pandemic, with face-to-face assessment only recently introduced. At the time, access to further mental health assessment was prioritised to those considered most urgent as a necessity. In the early days of FRS, there were other services involved in triage of referrals and assessment, Initially there was confusion as to which team was taking referrals. This has now been resolved.
10.3 Managers of supported living services described relying on information and assessments from mental health services before placements were made. Reflection on events concluded that without the correct level of support from mental health, supported living for people with complex mental health needs could not be provided. Providers have introduced placement panels with their own experienced staff, which enables further exploration of the application, discussion with the individuals and services making referrals to get a better balance of information and risk. This was not only because of events with Adult C and B, but because of other experiences where access to mental health support was not forth coming. Supported living and adult social care staff spoke about feeling left on their own with very complex and distressed individuals and feeling totally out of their depth.
10.4 In contrast to views from agencies about the need for a support and consultation service, Devon mental health services commented on their inability to meet all perceived needs. There remains an ongoing challenge to balancing all demands on local mental health services. DPT identified a disparity in their funding, and commissioning compared to other similar areas, and in comparison, with funding to physical health care. The ingredients of the pandemic, staffing absences, recruitment difficulties in mental health (as experienced nationally), number of mental health social workers, and less inpatient beds per population compared to other similar areas, influenced how care was delivered and experienced by the three men. The continued need to prioritise urgency impacted on clients open to services. Those individuals receiving support via other commissioned services had their changing needs balanced alongside the referrals with no support, and urgency of these required prioritisation. Mental health commented that those who do not meet the threshold for detention under the Mental Health Act have a choice to engage with advice and options offered.
10.5 Devon as a county is bordered by two unitary authorities: Torbay and Plymouth. Devon County Council have assigned social workers who provide mental health services whilst Torbay and Plymouth have made alternative arrangements. Mental Health Social Workers in Torbay remain employed and accountable to the Integrated Care Organisation (TSDFT) but are co-located with their DPT colleagues. Access to Mental Health provision however follows the same procedure and eligibility as used by DPT in Devon which means unless there is an immediate need for Mental Health Act assessment, a person must have a referral via their GP and have an identified secondary health need for Mental Health services before allocation to the most appropriate professional is progressed.
10.6 Within Torbay adult social care, adults with packages of care are given an annual review, or review when circumstances change. The adult social workers who know the person well are usually tasked to undertake the review. Risk assessment informs how social work is allocated and there is ‘active case management’, for those people who require interventions currently. Adult B’s care was managed in this way.
10.7 There were a number of referral points in agencies and services with the same or similar title and acronym. An example of this was the single point of access (SPA), in mental health services (prior to FRS). This was the access point for referral and triage into mental health services. There was at the same time in Torbay and South Devon NHS Foundation Trust the Single point of contact (SPOC) for adult safeguarding referrals. Raising an adult safeguarding concern had a number of options, dependent upon what local authority area it was, Torbay and South Devon, Devon and Plymouth. These local authority areas have separate boundaries and from discussions this created confusion at times, in this review and in others. There appears to be current discussions about the number of local authority boundaries and whether these could be drawn together in the future.
11. SAB Leadership oversight and governance – Torbay and Devon Safeguarding Adults Partnership Board (TDSAP)
11.1 There were challenges encountered in the SAR process, with considerable time delays in accessing information from a number of key agencies. Although the SAR template clearly states additional information may be required and requested, the LR was dependent upon information the services involved were prepared to provide. These problems were escalated to the Partnership, and throughout, the LR was professionally and courteously supported.
11.2 Many of the difficulties encountered were pandemic-related, and due to the passage of time since the deaths. The pandemic led to increased pressure on services which in turn led to agencies having limited capacity to respond to requests for additional information, and there was an inability to release staff for interview. The ambulance trust informed the TDSAP Board that they were unable to respond in detail to every SAR due to the wide area covered and the number of SAR requests. Adult social care was delayed in responding to specific questions due to the demand on staff and limited time to review records. There was also a nationwide IT outage that prevented access to mental health electronic records. Additionally, some IMRs were of poor quality, and not all services involved were identified, and their IMRs were not requested. The Board previously identified the quality of some IMRs as a weakness, and there are plans in place for the development of an IMR podcast which would support practitioner learning for completion of these.
11.3 The SCiE SAR quality markers (Appendix 6) were used to demonstrate governance and transparency of the report. Two quality markers were only partially met, these were markers for ‘assembling information’ (QM9) and ‘practitioners’ involvement ‘(QM10).
11.4 In the LR’s experience, when conducting such reviews, there is typically a procedure in place to access agency information that enables independent assessment of material. This process allows for clarification of facts and helps avoid internal agency bias. In this SAR there are examples where agencies had included information that significantly differed to that of other agencies accounts. Although a degree of variance is expected, what was unusual (in the LRs opinion) was the inability to independently gain clarification from records.
11.5 The SAR templates provided were comprehensive and clearly outlined the information required from agencies. One observation made while using the material was that it would be more helpful to have the name of the agency in full, followed by the acronym, the name of person and role at the head of the template. This would allow for the agency, person, and role to be easily identifiable before reading the content. Although this information is available at the end of the form, the LR believes it is beneficial to have this at the head of the document.
11.6 The Care Act 2014 mandates Safeguarding Reviews and requires agencies to cooperate. Acknowledging the current and significant pressures, cooperation is vital to ensure that reviews are meaningful to both adults, their families, and future prevention. This raises uncertainties and challenges going forward in how TDSAP can attain the expected level of engagement from all agencies involved, balanced against the demands and pressure on services.
11.7 Since the deaths, there has been transformational and ongoing developmental work in mental health services for adults and older people. To acknowledge the passage of nearly three years and taking account of this, the recommendations focus on providing assurance to TDSAP that themes and system issues identified in this SAR have been addressed.
12. Conclusion
12.1 The analysis and observations in this SAR are made with the advantage of knowing what happened from each agency perspective and looking at the situation as a whole. Understanding what happened and why requires awareness of the local rationality of professional practice, how people were making sense of an evolving situation at the time. Local rationality helps understand the thought processes and motivations behind decisions and actions, how the circumstances looked to someone in the moment. What the world looked like to those involved will differ according to various factors including what information was available to them, what was capturing their attention, what knowledge and experience they drew on to make sense of things, the goals they were trying to achieve and the conflicting priorities they were juggling.
12.2 The care and support of the three men occurred during the unforeseen and unprecedented global event of the pandemic. There is no doubt that the pandemic had an impact on the experience and level of service delivery at the time of the men’s relapsing mental health and ongoing distress. Most services and agencies had face to face contact with these men in the normal course of their working activities. However, the vital central service of mental health was impeded by the pandemic and other local factors, requiring services to continually prioritise urgency of all demands. Mental health contact was primarily provided through telephone and short visits, with reduced attendance at supported living premises. Risk was mitigated by perceived protective factors. Practitioners made decisions based on what was known and knowable at the time, taking account of previously understood information. Working within the restrictions of the pandemic reduced the ability to understand the full set of events, as different perspectives of the same event were pivotal to the situation. The LR concludes that if access to mental health services had been easy and comprehensive, it cannot be known if outcomes would be different. This SAR identified that the voices of the men and practitioners struggling to support them were not heard, and agencies reflected they were not working in a united partnership.
12.3 The LR appreciates the help and assistance provided by staff and managers of the various services, and acknowledges the challenges of working with these men, and the staff commitment in continuing delivery of services during the pandemic.
13. Recommendations
In response to the following recommendations Torbay and Devon Safeguarding Adults Partnership (TDSAP), will develop an action plan with time scales, that are realistic and achievable with partner agencies.
The recommendations are made considering the length of time elapsed since the three men died, the ongoing service development work in mental health services, and recommendations made in other recent SARs, avoiding repetition of other ongoing actions.
The recommendations aim to provide governance and instil confidence by means of assurance that service development and changes made in mental health services over the last few years has addressed the identified system issues and gaps.
Recommendation 1
The ICB and DPT provide governance assurance to TDSAP that the outcomes of the service development in response to the Mental Health Framework, have addressed system issues and closed the gaps identified in this SAR. (see below)
Gaps identified.
- Mental health support to GPs, other commissioned services and supported living,
- Delayed communication to GPs, support with prescribing for mental health conditions.
- Information sharing with agencies and commissioned services.
- Flexible approach to service criteria, see the whole person and co-production at time of crisis for people with both mental health and learning disability.
- Multiple responses to mental health crisis by ambulance and police. Consider new models of working in partnership with emergency services in response to mental health crisis and self-harm.
- Limited family involvement
- Consideration of mental capacity, decisional and executive capacity.
- Risk assessment.
Mental Health Framework developmental work addressing these gaps described as:
- Dedicated functions of mental health personality disorder and rehabilitation services have explicit responsibilities to provide advice and guidance to supported living, and other commissioned services.
- Primary Care Networks (PCNs) hold multi agency team meetings to discuss patients with unmet needs and care pathways are identified.
- PCN’s have mental health clinicians via the Additional Role Reimbursement Scheme (ARRS), providing support to Primary Care and the interface between Primary and Secondary care.
- Developmental plan for single trusted assessments which identifies the right pathway for people and builds a care package around what they want and need – the interim vision for ‘No wrong door’.
- Dedicated FRS line for police to use to access mental health assessment for section 136 and other advice, implemented September 2023.
- Improvements in the quality of risk assessments / training
- Increased Family involvement, Stronger together – families and carers
- Mental capacity – assessing and application, recording and need for training.
- Working with personality disorder
Recommendation 2
TDSAP include in data collection, quarterly information about numbers of suicide and self-harm deaths in the local population, and for people using mental health services. Data from partner agencies to include themes and learning from reviews.
The purpose of this data:
- TDSAP has an ongoing awareness of the numbers of suicide and self-harm deaths in Devon and Torbay.
- Provide ongoing assurance that themes and learning from this SAR are not repeated in other suicides/self-harm.
- Enable multi-agency analysis of themes and learning, with identification of action required by agencies, or the partnership.
Recommendation 3
TDASP facilitate development of a multi-agency urgent escalation protocol that includes senior leadership, with decision-making authority, in circumstances of mental health crisis and agency disagreement. This protocol will be used when the concern does not meet the threshold for the safeguarding escalation policy.
Recommendation 4
The ICB and DPT review the effectiveness of ED and liaison psychiatry communication to agencies and GPs about frequent attendees at ED with self-harm.
Recommendation 5
The ICB, Ambulance Trust and ED services review the handover process for information, to improve information sharing of disclosures made at attendance with patient, prior to admission to hospital.
Recommendation 6
DPT review how Adult N personal and mental health history was collated to determine how important mental health history was not available to the clinical risk assessment. Produce an action plan to prevent reoccurrence.
Recommendation 7
TDSAP make minor revision of SAR templates to include.
- Full name of agency, acronym, and name and role of person completing at head of document
- Prompt for agencies to record other commissioned services and contact details of these services.
- Glossary of agency acronyms.
Recommendation 8
TDSAP advise agencies / organisations involved in a SAR to make available when required (as a minimum) the last 3 months of agency records about the adult for clarification and fact checking.
Recommendation 9
The ICB to review the inequalities in the funding and mental health inpatient bed provision in Devon compared to other similar populations. Establish a rationale for the differences and discuss a way forward to address these issues.
Recommendation 10
DPT to address the additional family questions about Adult C in a meeting with the family, clinical team and consultant psychiatrist.
Glossary
SAR Safeguarding Adults Review
TDSAP Torbay and Devon Safeguarding Adult Partnership
DoH Department of Health
DPT Devon Partnership Mental Health NHS Trust
SCIE Social Care institute of Excellence.
QM Quality Marker
LR Lead Reviewer
ADASS Association of Directors of Adult Social Services
SAB Safeguarding Adult Board or Safeguarding Adults Partnership
SW Social Worker
IMR Internal Management Review (Report)
ABE Achieving Best Evidence interview.
ED Emergency department
LD Learning Disability
NCISH National Confidential Inquiry into Suicide and Safety in Mental Health
MSP Making Safeguarding Personal
CID Crime Investigation Department
KE Key Event
DIY Do it Yourself
ECT Electro Convulsive Therapy
GP General Practitioner
CRHTT Crisis Resolution Home Treatment Team
DGH District General Hospital
MHA Mental Health Act
RCA Root Cause Analysis incident review (NHS)
SPOC Single Point of Contact
MHAT Mental Health Assessment Team
AFRS Access and First Response Service now FRS – First Response Service
PDP Potentially Dangerous Persons
MAPPA Multi Agency Public Protection Arrangements
NSPCC National Society for the Prevention of Cruelty to Children
PALS Patient Advice and Liaison Service (NHS)
ViST Vulnerability identification Screening Tool
ACE Adverse Childhood Experience
PTSD / CPTSD Post Traumatic Stress Disorder / Complex Post Traumatic Stress Disorder
OCD Obsessive Compulsive Disorder
IIOC Indecent Images of Children
PCN Primary Care network
CMHF Community Mental Health Framework
ARRS Additional Role Reimbursement Scheme
IAPT Improved Access to Psychological Therapies
LTP Long Term Plan
SPA Single Point of Access
AMHP Approved Mental Health Professional
ICB Integrated Care Board
Appendix 1
TORBAY AND DEVON SAFEGUARDING ADULTS PARTNERSHIP
GENERIC TERMS OF REFERENCE
The purpose of a Safeguarding Adults Review (SAR) is neither to investigate nor to apportion blame. The SAR requires outcomes that:
- The review process focuses on emerging themes and not reinvestigation of individual incidents.
- Establish what learning can be drawn from circumstances of a case in which professionals and agencies work together to safeguard adults.
- Identify what the learning is, how this should be acted upon and what is expected to change as a result.
- Review the effectiveness of procedures both of individual organisations and multi-agency arrangements.
- Improve practice by acting on the findings and developing best practice across organisations.
- Improve inter-agency working to better safeguard adults.
- Make a difference for adults at risk of abuse and neglect.
SPECIFIC TERMS OF REFERENCE FOR THIS THEMATIC SAR
1. Consider learning and themes from national suicide annual report 2018, and any local male suicides in the last 3 years and whether these apply in these cases.
2. Identify factors in the work environment that support good practice, and those which create unsafe conditions in which poor safeguarding practice is more likely.
3. How are services addressing needs of this group of men? What is available? What is working well? What are the barriers to addressing needs?
4. How are services working together? What is working well? What are the barriers to working together?
5. What do we need to do to improve support to this? Which services are engaging, which services are missing?
6. How are services working to engage people who present with distress and active thoughts about suicide, how person centred and flexible is their engagement approach?
7. Did the agencies involved in each case, consider trauma awareness and understanding?
- If so, did they recognise the signs/symptoms of trauma for each person and in working with the person, acknowledge the impact of traumatic experiences from the past.
8. Establish whether there are service-related themes or wider issues or links recurring across the three cases, for internal learning and action for individual agencies.
Appendix 2
CHRONOLOGY OF EVENTS – ADULT C
This section includes the key events (KE) generating questions for analysis, missed opportunities and the emerging themes and findings.
October 2019 – C remained distressed and had contact with mental health services and police, with thoughts of self-harm, statements made that he can no longer go on. C took himself to local cliffs on several occasions with statements about his intentions to jump. C called services to verbalise his suicidal thoughts and distress, this is described as ‘self-rescue’– alerting services to his distressKE1. C was assessed at ED by Liaison Psychiatry, he expressed dissatisfaction with life and inability to manage activities, he also talked about the future and employment and getting a dog.
November 2019 – Early November (7th) adult C was admitted to ED by ambulance. C was “acutely confused and unable to walk”, he was experiencing alcohol withdrawal.KE2 On discharge (18th) C went into supported respite accommodation with support from CRHTT after threats to hang himself if he went home. There were concerns about self-neglect, and severe depression with some psychotic symptoms, including a preoccupation about his bowels and that medication had damaged his brain. C thoughts were described as almost delusional in their intensity. C was unable to listen or accept reassurance.
December 2019 – Referral to social care for supported living. C was described as experiencing depressionKE3 and dependant personality disorder. Background information provided included – relationship breakup, self-neglect, confused state, alcohol withdrawal and recent detoxification, high risk of suicide, threats to drive his car to end his lifeKE4, and psychotic thinking. Respite supported living found C was independent with personal care and mostly self-sufficient practically with prompting but very demanding emotionally on staff – seeking reassurance about every twenty minutes. The Respite stay was extended due to risk of harm if he went home. C had a Mental Health Act (MHA) assessment after deterioration and refusing medication. He agreed to take medication when this was reduced to a minimum, therefore he was not detained. Upon discharge from CRHTT on 17th, C was more settled and doing physical activity, needing help with emotional support and direction to plan his day. C decided not to return home as too many painful memories. Late December the GP thought that C was delusional about taking anti-depressant medication.
January 2020 – Mid-January (18th) C was doing well but has concerns about his medication and the numbing feeling. He was changeable about supported living. He had ten hours of one-to-one support to help daily motivation. C was considering work via employment support. C said he had thoughts about jumping off cliffs several times. C expressed a concern that he may have dementia in late JanuaryKE5
February 2020 – Throughout this month C is expressing distress, he was not coping emotionally, and had intrusive thoughts to drive his car over the cliffs, he disclosed to supported living staff that he would “rather be dead than live like this”, and that he could see no future and wanted to end his life by jumping off a cliff or in front of a trainKE6. C responded to direction, but decision making was difficult. C disclosed suicidal thoughts to the social worker, and he was signposted to the duty CMHT worker. Supported living staff record C statements about killing himself and there was a question whether this was an attempt to get more one-to-one timeKE7. A CMHT multi-disciplinary team (MDT) meeting took place – C was observed to be highly agitated, distressed, and dependent on staff. Additional medication for anxiety to be taken when needed was prescribed.
March 2020 – During March there are continued high levels of distress and anxiety. C went to the cliffs and then rang staff for assistanceKE8. C stated, ‘my brain is sliding away, and my brain is gone’. C also attended ED as he wanted admission. At the outpatient appointment C told the consultant he believes he has dementia or physical problems; and a brain scan is agreed to provide assurance to him. At the start of the pandemic, C left the respite placement and returned home suddenly, initially there was no support package and C was alone. Support was set up two days later. C struggled with the support, remained distressed and made multiple calls a day to the care coordinator.
April 2020 – KE9 C continues to express high levels of distress and suicidal thoughts and acts of self-harm. C took a significant overdose, and he attached a belt around his neck as a noose and stated he intended to hang himself from the door. C continued to make threats to harm himself and described hearing noises in his head. C was found standing on the edge of the cliffs and the public phoned emergency services. C made multiple calls to street triage, this was documented as a means to accelerate services, he also called the ambulance twice within twelve hours. C was assessed in the mental health hub and seen in ED by liaison psychiatry, after repeated calls to services with threats to cut his wrists. C repeatedly requested hospital admission as a means of stopping him wanting to end his life. The enabling one-to-one support was increased in response to the continuing distress. C is unable to do tasks and does not know what to do most of the time, feeling overwhelmed, C does not feel he is improving with enabling support and supported living is agreed.
May 2020 – Referral for supported living. C had another scan of his brain, showing evidence of the previous stroke, some cerebral atrophy, more than would be expected for his age, but no significant change to the scan in 2017KE10. C was not reassured by these findings. In late May, C called FRS to say he had cut his wrists, and an ambulance conveyed C to hospital.
June 2020 – Initially there is some improvement in C management of activity of daily living, but C cannot recognise this and continues with circular conversations about the same topic. C continues to be severely distressed, and change worries him, he was fixated on medication and his body not working, he struggled with concentration. The possibility of autism is considered due to his fixed beliefs about medication, and an online assessment is requested. The GP was struggling with numerous calls from C to the surgery and his non engagement with medication. C went to the cliffs again and calls staff to say he was two feet away from the edge and wanted to jump, the social worker ‘talks him down and away from the cliff’. C goes back to the cliffs a few days later and is found with his legs dangling over the edge. There is more self-harm, an overdose with alcohol, and during assessment C was preoccupied with his ‘brain not thinking and working properly, that his medication was affecting him, and no one was listening’, C makes multiple calls to the ambulance service. There are two increases in one-to one hours agreed in C best interests as he appears not to have mental capacity to decide this, 21 hrs. and then 28 hrs. There is another CMHT discussion about C and management, and supported living is agreed as the way forward. At assessments C was confused and he admitted to stopping his medication. After one assessment, police are called because C is refusing to leave, and he was getting aggressive. Respite funding is not agreed because C was in mental health crisis,KE11 and therefore this is not a social care need. C then stopped engaging with the one-to-one support and went to stay with friends. The Care agency end their contract due to non-engagement and the demand made on service. The supported living placement was asked to fast track the placement arrangements due to his mental health needs increasing.
July 2020 – C continues to be severely distressed and agitated during July. There are two mental health assessments, Liaison psychiatry x 2 after an overdose, and an episode where C called the ambulance because he cannot breathe and has extreme anxiety. C was given diazepam, and his physical observations were within normal ranges. He told staff “I came here for help” “You cannot keep sending me away” and “I want hospital admission”. There is a review with consultant psychiatrist and care coordinator at home. C stopped taking his medication as it was not working, he reports he thought he had a learning disability as it took him time to learn new things. A re-referral to respite care was declined as C was unable to state he would be able to keep himself safeKE12. C was at home with no formal support and supported extensively by his friends for a short period. Mid-July (13th) C was prescribed an antidepressant, a benzodiazepine to calm anxiety and medication at night to help sleep. C was really struggling at this point, hardly sleeping despite long walks in the day. C again talked about a feeling that something was wrong with his brain which needed to be fixed. On 20th, C moved into supported living, which necessitated a change of CMHT with a 3-month transition period. There was a telephone call with the care coordinator, who notes that C was fixated on his brain not working, and how he wanted to get back to how he was. On the same day C abandoned his car and was reported as a high-risk missing person. He was located by police at a local area with radio masts, and concern was expressed about Cs reason for going to this location, following threats to jump from cliffs. C then begins to settle in supported living, and his anxiety and distress is less. The care coordinator contact is then reduced to three weekly intervals as he was initially settled. After the short period of settled behaviour, C’s distress and anxiety starts again. There were then numerous contacts with FRS and Single Point of Contact (SPOC), and CMHT duty desk, as C was phoning dozens of times during July.
August 2020 – Throughout August, C continues to be distressed and his mental health continues to deteriorate. Supported living staff feel C was destructive from the outset, causing issues with fellow residents. His needs impacted on time allocated to other residents. Staff suspected alcohol use, this was smelt on him, but staff had no powers to prevent alcohol use.KE13 There are a range of concerns expressed by supported living staff to mental health services, and to the care coordinator. These were described as C having incidences of ‘vacancy’, his eyes not having any focus with self-escalation of anxiety, and C had stopped medication. C phoned FRS, in calls he is described as giving delayed and incongruent responses to questions, and low and flat in his mood. FRS lead was consulted and the decision made that a referral to CRHTT was not indicated, as C had a good package of care in place.KE14 The supported living staff expressed dissatisfaction about the plan and requested additional support hours. FRS also had contact with paramedics and supported living staff about C. It was necessary for C to be isolated from other residents due to his behaviour, he was pacing and highly agitated. Other residents were distressed. On 13th, the CMHT had a telephone phone call from the supported living service manager who was concerned about C demand on staff, distress caused to others and that his care hours needed urgent review, C was continuing to refuse medication, he was fixed on the same thoughts and sentences, struggling to engage, struggling with the shared care hours. It was reported that C had grabbed a member of staff, there were concerns that staff were ‘burning out. C had an incident of exposing his buttocks and he seemed to have lost social skills and was entering other residents’ rooms. More one-to-one care hours are suggested, with a request for two additional hours each day one-to-one care. The social worker was unable to action this prior to C’s death. In a video appointment with CMHT consultant psychiatrist and care coordinator, it was noted that after good start, C had deteriorated around 8th August and this deterioration continued. C was refusing medication and was increasingly agitated. An urgent GP letter was sent to change medication after an error is noted. The outcome from the video appointment was that medication is changed from Sertraline to Mirtazapine, care coordinator to remain in touch with C and supported living, the consultant would review again in six weeks. It is also recorded that at this review, C appeared more kempt and relaxed than before his move. On 14th the supported living staff record C was agitated and assaulted care staff. C was refusing medication and was very confused, grabbing hold of staff.KE15 Support staff report there was almost an immediate deterioration in C’s mental health with the change of medication. In late August (25th), C had second trial day at charity shop, which did not go well, and C was asked not to return. On 28th, there were difficulties with C insisting he was going to drive to his daughters’ home in Hampshire, despite the DVLA being notified about concerns re his fitness to drive. Support staff tried distracting C, who was agitated and distressed. By the end of August (31st), C was obsessively saying he wasn’t getting any better, and was aggressive in his communication and frustrated he couldn’t drive.
September 2020 – Mental health distress continues. C is frustrated because he is not able to drive, advice was given to support staff to call police if C tried to use his car. C called an ambulance – he believed his body was not working, he was unable to pass urine for two days and was constipated for four days. After liaison with the GP, C was taken to ED for assessment. C was dehydrated and constipated; treatment was given. Medication recently started had contributed to this. C is increasingly agitated and stressed about his health throughout the day repeating “I’m dying, my body is not working, I can’t wee or poo, I can’t sleep, I may as well just jump off a cliff”.KE16 Staff tried to reassure him that he was okay physically, with no effect. On 3rd, C was having difficulty accessing online banking; C trying to transfer all his money to his daughter as he said, “he didn’t need it anymore”.KE17 He was adamant that as he was dying, he did not need the money, then Support staff report his mood was settled later that evening. On 4th, the day of death, C contacted an ambulance at 05:39 hrs. C was distressed and felt his body was not working, and that there was something wrong with his genitals. C showed ambulance staff his buttocks and informed them he could not pass urine. Support workers informed the crew of previous hospital attendance and advised was C eating a drinking normally, and the toilet heard flushing in the night. Ambulance crew left to attend another urgent call, and further ambulance sent to assess C, arriving at 06:09. Support staff tried reassuring C, reminding him he was eating, drinking and toileting normally. After reassuring C no physical symptoms could be found, the ambulance crew informed the GP, and made a referral to adult social care for safeguarding, self-neglect, and concerns about C being a frequent caller. C remained at the home with the staff. Adult C was anxious and agitated, stating he was dying; he spoke about ending his life and left the accommodation in a taxi. C was then reported as a missing person and located by police. Upon return around 10:30 hrs, C was pacing around and becoming aggressive in manner. Staff were concerned about his behaviour and asked the police officer who had brought C back, to stay at the home while staff contacted mental health services for an assessment. Staff called the CMHT and were advised C was still under the care of the previous team and to call that team. Staff had a forty-five-minute telephone call with CMHT and were advised to refer to the GP. In a conversation with the CMHT Duty Worker, C stated he felt the decline in his mental state was related to re commencing Mirtazapine two weeks earlier; the supported living staff agreed and ‘both felt he was more stable on Sertraline’. The CMHT consultant psychiatrist advised of the history of dissatisfaction with whatever medication was prescribed and that C had done well on Mirtazapine in the past. The psychiatrist commented that C needed to stick with one anti -depressant medication, for prolonged period to assess its benefit. The Police officer had to leave, and staff contacted the GP for an emergency call back. The Home’s senior manager was notified, and C was making himself something to eat and had calmed down. In the early afternoon,12:50 hrs, C left the accommodation telephoning staff he had a GP appointment at 13:00hrs and was going to walk to the GP surgery. At 13:35hrs the GP called from the practice and agreed to prescribe diazepam for C. Staff enquired if C had attended his appointment, and the GP informed the home that C did not have an appointment. The GP was concerned after staff made him aware that earlier in the week C had transferred all his money to his daughter’s bank account, possibly this was an indication C was ‘putting his affairs in order’ prior to taking his own life. The GP advised staff to contact police urgently. When C left to go to the surgery, he was calm and lucid, he made no mention of wanted to end his life. C’s personal emergency plan meant that after one hour of being missing staff should contact police, but staff acted more quickly due to the conversation with the GP. C took a taxi to the cliffs where he then jumped. There was a note found in his belongings on the cliff addressed to his children, along with an empty bottle of wine. Three days after the death (7th) the referral from the ambulance service for safeguarding, self-neglect and frequent caller was received by adult social care and interpreted as welfare support. The referral was immediately sent to CMHT as there was an identified mental health worker and the person was experiencing a mental health need.
KE1 Staff interpret C actions as self-rescue that of alerting staff to his distress, seeing his actions of threats of suicide through the lens of dependant personality disorder and the protective factors of a package of care.
KE2 alcohol use information is limited, but appears to be an issue for Adult C
KE3 focus of information is on dependant personality disorder, although witness statement to coroner states treatment resistant depression and dependant personality disorder traits
KE4 risk assessment, statement of intent, method, psychotic thinking observed.
KE5 there was no information to show discussion with C about dementia in the information provided to the SAR to explore this.
KE6 risk assessment – statement of intent which includes method.
KE7 threats of self harm seen through the lens of personality disorder and attention seeking
KE8 seen as self-rescue in assessment of risk
KE9 April 2020 has self-harm attempts, there is a perception about using self-harm to accelerate service responses.
KE10 C is concerned he has dementia
KE11 There is recognition here that this is a mental health crisis.
KE12 C unable to state he will keep himself safe – notion of commitment of keeping self-safe is unreliable, similar to suicide prevention contract – an agreement not to die by suicide is written into the contract. Suicide prevention contracts have been shown not to be effective and considered an “overvalued clinical and risk-management technique.” It has also been argued that contracts introduce coercion into therapy.
KE13 alcohol use is a continuing problem which was not assessed further, from information provided to the SAR.
KE14 This is a key factor in adult C risk assessment which was misleading, and minimised risk as staff saying they could not manage C behaviours.
KE15 C refusing medication and very confused, mental health relapse
KE16 levels of despair and statement of intent of suicide with method identified.
KE17 C is putting his affairs in order which was a risk flag when reported to the GP
Appendix 3
CHRONOLOGY OF EVENTS – ADULT N
This section includes key events generating questions for analysis and identifying missed opportunities and the emerging themes.
August 2020 – This is a significant month, with a number of self-harm presentations at ED with overdose of paracetamol with alcohol and his mother’s medication.
15th Aug – N consulted his GP about low mood, and poor sleep. Suicidal thoughts were denied. The GP prescribed anti-depressant and medication for insomnia. N had ED attendances via ambulance on 16th, 20th, 22nd and 24th August after an overdose.
16th Aug – Disclosures were made to ambulance crew and include anxieties about the pandemic and his mother, this was a cry for help and overdose was partly because he wanted to die,KE1 N was concerned that he had no internet, he was very lonely, he was drinking more and not eating. N is assessed by liaison psychiatry, N said he felt suicidal intermittently and spoke about his increased alcohol use, N also disclosed an overdose several years ago.KE2 on subsequent attendances N declined assessment.
20th Aug – N says he was struggling with a recent break up, and that he did not want to ‘wake up’KE3, from the overdose, N was ‘fed up with life and caring responsibilities’, he did not want to die and was keen to go home.
N also had telephone consultation with GP about overdose, excess alcohol and the medication prescribed by GP. N spoke about anxiety but denied suicidal thoughts. N told GP he was taking medication, and it was already helping. The GP thought N sounded well and was not voicing suicidal thoughts. N advised follow up with GP in one or two weeks to review his mental health.
22nd Aug – N took an overdose instead of using contact details for services to help him, he wanted to go to sleep and not wake up. N said the amount of alcohol consumed was 4 litres of cider and he confirmed he had suicidal thoughts. Liaison team is short staff and FRS triage N via telephone call and decide he does not need to be seen face-to-face.
24th Aug – N was not taking medication prescribed by his GP after reading the side effects.KE3.3 N acknowledged his behaviour was out of character and he was drinking more than normal. In ED, N gave contradictory information to staff. N said his overdose was a spontaneous decision and he was unsure why he did this, he regretted the overdose and wanted to sleep. N does not know why he took an overdose, he said he has no suicidal thoughts and regrets taking overdose and wants to go home.
N is offered assessment by Liaison Psychiatry, but he declines this,KE4 saying he was assessed on last attendance, which is not the case. N offered assurance that he would use the help line numbers. Discharge plan is the notification to the GP and referral to alcohol services.
28th Aug – GP appointment, N told staff he was ok, and cancelled the appointmentKE5.
5th Sept 2020 – N took another overdose, fifth one. When N was in ED, he stated he does not know what triggered this one, he described generalise anxiety, his mental health affected by lockdown. N said he was ‘better out of it and had considered taking his own life’, no plan disclosedKE6.
Ns mother was concerned was self-neglect, N was not eating properly over the last month. N explained a history of deteriorating mental health and N is recorded as ‘high risk’ on the nursing mental health assessment.
N spoke about feeling isolated with no social network and finding lockdown difficult. After blood results, N was allowed home with ‘safety netting’, described by ED as the mental health plan as per the mental health team, agreed with N, that he will seek help from services / GP.
8th Sept 2020 – A referral was made by Liaison Psychiatry to alcohol services, and N was contacted the following day. N declines the assessment againKE7.
11th Sept 2020 – Two days later his mother found N suspended from the banister deceased.
KE1 N wants to die – statement of despair
KE2 significant mental health history known to GP but appears not known to mental health services.
KE3 consistent statement of desire to die.
KE3.3 refusal of treatment not taking medication – was this communicated to GP? ED were also informed of this.
KE4 missed opportunity to assess N, and N information was not accurate – refusal of services.
KE5 further refusal of services – GP appointment to follow up mental health.
KE6 ED record 5th overdose and note N has no plan, however he is taking overdoes, is this considered as a plan?
KE7 more evidence of refusal of services – self neglect
Appendix 4
CHRONOLOGY OF EVENTS ADULT B
This section includes the key events generating questions for analysis and identifying missed opportunities and the emerging themes.
October 2017 – Adult B had his first contact with adult social care. Assistance was provided to support B to move, as the then carer was no longer able to offer their support. A supported living facility in Torquay Devon was found.
May 2018 – Adult B moved into his flat in a supported living environment with daily input for support.
August 2019 – A significant deterioration in adults B’s mental health was observed, and concerns were raised with the GP, Adult Social Care, and the mental health service. B made a disclosure to support staff about his “inappropriate thoughts about children and he was stopping himself from harming others, that he had had enough, and that he wasn’t right in the head and that he was going to hell, B wanted to drink himself to oblivion”KE1. An ambulance was called, B was assessed by psychiatric liaison at the Emergency Department (ED). Adult B shared a range of concerns, that he did not like supported living, he was feeling scared and had been having suicidal thoughts on and off for a long time, that he had thoughts about stabbing himself, thoughts about abusing children, and he reported gambling in his spare time. He also made a disclosure that he was looking at child images on his computer. Adult B had started drinking, and smoking, both which was out of character.KE2 Staff were concerned about B’s risk to children when under the influence of alcohol. During assessment B disclosed he was having thoughts about harming others but had stopped himself as he did not want to harm anyone. Adult B was assessed as safe to return home as he had a package of care, and a referral was made to CRHTT for a medication review. The self-disclosure about child images was passed to police, and his computer was seized for investigation. The adult social worker who knew B well noted that this was the start of deterioration in B mental health, with increased obsessive behaviour and self-isolation. Mental health and supported living staff believe the police investigation is increasing B’s anxiety.
Aug – Dec. 2019 – Police completed a ViST recording their vulnerability assessment and B was referred to adult social care due to mental health deterioration. B was assessed by liaison psychiatry at the local ED in September when B presented with significant physical health difficulties. B was assessed again by liaison psychiatric in October for depression and a change in medication was potentially a contributory factor in his decline in mood. B was also self-isolating in his flat more. A risk enablement meeting was held in October. B was involved in this process and one-to-one hours were purchased to held B participate in community activities to reduce his isolation, i.e., a computer course. Adult B contacted the GP several times in December, about increased anxiety, and the GP referred B to mental health services. It was also noted during this time that B was not accurate recording his blood sugar levels.KE3
January 2020 – B was admitted to ICU with oesophagitis.KE3.1
February 2020 – the GP referral led to an assessment by the Mental Health Assessment Team (MHAT). In this assessment it is considered B’s anxiety may be due to police removing his laptop after his self-disclosure of images of children on his computer.KE4. No illegal images were found, but B said it was ‘still on his mind’. B said he would ‘not hurt anyone’, and that he ‘did not find talking to people helpful’. In this assessment B disclosed he felt low in mood, and have done so for a number of months, with almost constant intrusive thoughts to harm children and adults. B said the thoughts around children were mainly sexual in nature. B said he preferred to isolate himself as he was frightened about going out due to the intrusive thoughts. B spoke about thoughts of ending his life, and had been thinking about suicide more frequently, but denied plans, his mind constantly racing, and he had intrusive thoughts about sexually and physically harming others. B disclosed he experienced auditory hallucination but was unable to discuss these in detailKE5. B was not observed to be responding to voices during assessment. Risk to self was assessed as medium – the thoughts to end his life were distressing, but he had no plans to act on these thoughts, but he was unable to identify any protective factors. B was socially isolated and did not like talking to staff about how he was feeling. He denied self-harm in the past, or an attempt to end his life. Risks to others was assessed as medium. B had frequent intrusive thoughts about harming others, B said he would never hurt anyone, or act upon the thoughts but was unable to identify protective factors. B disclosed that he had sexually abused others, including and a three-year-old girl when a teenager. Risks from others was assessed as medium. B was potentially vulnerable to others due to borderline learning disability, particularly if under the influence of alcohol. Talking therapies was discussed but B said he did not find this helpful. The assessment concluded that a referral to secondary services was not indicated as B was in receipt of a package of careKE6, and he did not identify anything other than medication that he would like support with from mental health services at present. Some online and community resources and contact information was provided to B.KE7
March 2020 – B was supported to apply for voluntary work to help with sense of purpose as he had experienced in the past. Police confirmed the outcome of their investigation, that there was no evidence on his computer of illegal child images. The police may want to interview B re self-disclosed assaults on identified others when a teenager. B continued to verbalise to support staff about thoughts of suicide by jumping off balcony.KE8 Support staff gained B’s permission to lock his balcony door, and his medication was checked to see if he was taking this properly, the GP was contacted, who suggested B talk to out of hours drop-in mental health support, or the Samaritans. The adult social worker who had knowledge of B visited and communication aids were offered and declined. B did not meet any specialist team criteria as advised from local mental health and learning disability services. An appointment with consultant psychiatrist for review and medication was offered. This appointment was then cancelled due to the pandemic and a letter sent to B recorded that mental health services had to concentrate on urgent cases that require immediate review, and therefore the team were not undertaking routine appointments for the foreseeable futureKE9
April 2020 – B was referred to the Access and First Response service (FRS) by his GP who is concerned about high levels of anxiety, thoughts of a sexual nature and that B was potentially a risk to himself or others. The referral was passed to the CRHTT who completed an assessment. Adult B spoke in assessment about intrusive thoughts and wanting to look at images of children – which was distressing, and he knew it was wrong, he felt agitated, could not cope anymore, and wanted to kill himself. B stated he planned to do this by stabbing himself. Supported living staff had removed knives from his flat, had locked his balcony door and removed the key to help keep himself safe. B spoke about OCD rituals, repeated washing of clothing, counting (avoiding number 7). B spoke about his abusive behaviour to staff at the accommodation, threatening them with a knife. B admitted to targeting staff and the staff had concerns about safety of B and risk to others. The GP was concerned because thoughts about harming himself with a knife are new. It is noted by MH staff from notes that thoughts about self-harm with knives was ongoing from last year. B was not able to access his usual coping strategies due to lockdown. B spoke about not wanting to live with these thoughts anymore.KE10
May 2020 – B was taken on by CRHTT, longstanding mood disorder with possible psychotic overlay at times with obsessive compulsive component and recent deterioration in mood is recorded. B received daily visits, and his medication was reviewed, after nineteen days B was discharged with conclusion that objectively B mood had significantly improved and there was a clear reduction in physical symptoms of anxiety and agitation. No psychotic or delusional symptoms were elicited at point of discharge, and B was referred onto CMHT.KE11 There was discussion between the HTT and the CMHT and it was agreed that B would be taken onto the CMHT case load. B was placed on waiting list on 27/05/2020.
June 2020 – CMHT staff made a home visit, B is noted to find it ‘difficult to engage in the conversation’. Following a multidisciplinary meeting at the CMHT, it was agreed that as B was unable to engage in the structured treatments offered, his care was transferred back to his GP on the 8th.KE12 The letter to the GP notes that B has borderline learning disabilities with possible diagnosis of Autism,KE13 and B had marked psychomotor retardation, poverty of speech, and he was very delayed in answering questions. An MDT discussion concluded that the team failed to see what B could be offeredKE14 and B had been in care all of his life, therefore team was discharging B back to his GP’s care. Later in June (22nd) the adult social worker is contacted by supported living staff, who were requesting additional support due to decline in B’s mental health. The CMHT were contacted and advised there was nothing they could support B with, and the GP suggested the adult social worker be notified of this. Towards the end of June (25th) Police completed a ViST[42] and sent this to Torbays Safeguarding Adult Single Point of Contact (SPOC) in Torquay Health and Social Care. Concerns noted on the ViST includes, general mental health is spiralling. There was an increase in B’s obsessive thoughts about sexual acts with children and although no evidence was found on his computer or phone of illegal images, police expressed concern due to the mental health deterioration and that his behaviour could escalate. The ViST notes there was an increase in suicidal thoughts,KE15 and B had disclosed information about numbers associated with violence. Police were requesting a multi-agency meeting. The Police referred into MAPPA and Triage concluded there were no adult safeguarding concerns.KE16 There was a re-referral made to adult social care due to safeguarding concerns from police who were requesting a multi-disciplinary approach. The adult social worker was advised that B did not meet MAPPA criteria but may meet Potentially Dangerous Persons Protocol (PDP[2]). B was then allocated to adult social care complex care waiting list.
July 2020 – The adult social worker who knows B is allocated setting up a multi-disciplinary meeting. The PDP referral form was submitted to police; however, B did not meet criteria for this process. The adult social worker liaised with the police about a joint visit to B. There were ongoing concerns regarding B mental health and suicidal thoughts were raised by supported living staff.KE17 B was offered an advocate to help him make a complaint about lack of access to mental health services and also a referral to specialist learning disability team, both of which B agreed to.
B’s consent was gained to share police ViST with ‘Stop it Now’ helpline[44], but he had difficulty accessing “stop it now” support. B was now experiencing a further decline in mental health, with an increase in suicidal thoughts, sexual thoughts re children and harming/staff/others, he reports he is struggling to control these. B was asking for help to manage these and does not want to harm anyone. As B was previously supported by the local mental health services CMHT, CRHTT, the referral was sent back to Mental Health Assessment Team (MHAT). B was also signposted to the NSPCC and the Lucy Faithful FoundationKE18. An advocate to help B was allocated on 17th. The referral to MHAT resulted in an agreement to attend a multi-agency meeting with adult social worker, advocate, police and representative from LD services and MHAT.
August 2020 – the adult social worker arranged an online multi-agency video conference. Adult B joined the meeting towards the end. It was agreed that mental health would do an assessment and the care package would be reviewed. Adult B distress as previously noted continued with same intensity. The LD forensic service advised that B did not meet their service criteria as has had no forensic history.KE19 In mid-August (14th) the GP contacted the CRHTT as B was expressing suicidal ideation but had no plans or intent. The GP made a request for the assessment by MHAT to be brought forward. The GP was advised the planned meeting on 8th September 2020 would still go ahead and to contact the CRHTT if B’s presentation significantly changed in the interimKE20 GP made a further request (20th) for the meeting to be brought forwardKE21 This was not agreed, and GP was advised to contact the HTT if B’s presentation significantly changed in the interim.
September 2020 – B distress continues, there is an escalation in threats to self-harm. A crisis visit is made by the adult social worker, who is now looking into other residential accommodation as supported living are not able to manage his mental health deterioration and escalating needs. There is contingency planning by provider to keep B and staff safe, involving calling for support from other supported living facilities. The GP is contacted about medication, B was deemed not to have mental capacity to manage his medication and was refusing staff to support him. The GP surgery phlebotomy team find B was more threatening than normal, and concerns were expressed about B attending GP surgery unaccompanied. CRHTT was contacted and difficulties with B talking over the telephone was explained. The adult social worker advised supported living staff to ask for a medication review at assessment. The GP contacted MHAT (2nd), via email – B’s main issue is described as his behaviour and frustrations of a sexual nature and comments about harming himself or others. The GP advised that the GP and supported living staff had ‘reached their ceiling of intervention’.KE22 The GP had advised carers to ‘ring the police and this was not supportive of the patient with learning difficulties and was reactive’. The GP was hoping MHAT would offer ‘urgent therapy and support to manage his frustrations, that all had a sexual theme’, and makes a notes of B own history of abuse. The GP states B’s needs are not being met. Adult B told the advocate he was self-harming and that he did not think talking about will help. MHAT assess B, (9th) at his flat with the advocate in attendance by telephone. The assessment outcome letter included that engagement was difficult, there was possible thought blocking. B needed significant prompting and responses were mainly one/two words. B stated he was having a “breakdown….his “past was catching up with him”, he had intrusive thoughts re harming children. B was unable or unwilling to discuss further. B knows this is wrong and was aware of the consequences of acting on thoughts. The assessment concluded that MHAT was unable to assess risk to children due to difficulty with engagement, assessment ended after 20 minutes with B and the advocates agreement, as B found it increasingly difficult to engage. Supported living is noted as protective factors, along with police knowledge of concerns about him.KE23 Recent self-harm with bruising was noted, and no clear suicidal ideation or intent is recorded. B’s distress was observed and there was acknowledgement of increased distress over 3 to 6 months. The risk to child was assessed as low, risk to B from others assessed as low, but acting oddly around children in public may increase this risk. The letter concludes thoughts of sexual activity was not a mental health diagnosis.KE24 B’s history was discussed with the team and consultant psychiatrist, it was concluded that engagement with secondary mental health care was not considered beneficial as B would be unable to engage with psycho-social interventions and may actually find this approach more frustrating than helpfulKE25 One-to-one time for daily activities were advised with a full physical health check to rule out physical health impacting on mental state.KE26 Medication was reviewed and changed, with medication for acute anxiety and agitation added. In Mid-September – a suitable respite placement was not found due to potential risks, and the adult social worker was exploring an increase in one-to-one support. The adult social worker visited B with the outcome of the assessment, and his care package was reviewed. This was a short visit as B was increasingly agitated.
October 2020 one-to-one support was increased. The GP practice sent a male paramedic (attached to the practice)[45] to monitor B’s blood sugars following concerns by the phlebotomist. B met the advocate and disclosed feeling hopeless, that he was stressed, low in mood and not sleeping well. B said he was willing to try the additional one-to-one support. B consented for the advocate to proceed with a complaint about lack of assistance from mental health services. In Mid-October (12th) one-to-one activity staff commence. B phoned the GP and disclosed an increase in anxiety and repetitive number counting. B remained distressed and was refusing two of his carers and was unable to give an explanation of why this was. The adult social worker saw B at home with the advocate and supported living staff for a review of his care. B was negative in response to suggestions made. The visit ended as B’s anxiety increased. B wanted more time to think about the complaint, a copy of the complaint letter was left for B to consider contents.
November 2020 PALS from the local mental health service acknowledged the complaint. B was more emotional and expressed he felt unwell. B needed encouragement to go out but did go out. PALS contacted B by telephone to gain more information. In late November B contacted the GP by phone and was extremely distressed. The GP phoned the manager at supported living and requested staff go to see B. Staff shared with the GP that B is like this every day and staff had contacted mental health frequently. Staff shared with the GP that there was nothing more supported living staff can do, they had been told to “get on with it”.KE27 The GP sent a text message to B advising him to take prescribed medication and that this is proven to reduce intrusive thoughts and behaviours such as the counting, reminding him that it was important for him to get up and out, to keep his brain and body active in the day, this was to help B sleep at night. B agreed to this advice.
December 2020 (8th) B contacted the GP surgery in distress, “I think I need the Crisis team” “I need to go into hospital” “I am having a mental breakdown” “I am thinking of doing bad things to *****” “I think I might have Alzheimer’s or senile dementia”. B finds it difficult to explain any of his statements. The GP made a referral to FRS – B was experiencing suicidal thoughts, ongoing obsessional thoughts of a sexual nature and high levels of anxiety. The adult social worker was informed of the referral, as this was passed to adult social care and was to be discussed at the multiagency meeting arranged for the 22 January 2021. Supported living now have concerns about road safety, activity staff have reported that B walks out into the road where there is moving traffic or lays down in the road.KE28 FRS advised they would ask if MHAT would complete another assessment. In Mid-December (10th), there was a face-to-face review meeting with B, the adult social worker, the advocate, and supported living. B feels things are deteriorating and he is feeling overwhelmed by intrusive thoughts. The GP and FRS both recommend further assessment by MHAT at this point. The GP contacted FRS (11th) seeking advice. Supported living staff are concerned that B has fallen in the gap between mental health and learning disability services. Supported living staff are struggling to manage B’s behaviour. FRS raised these concerns with MHAT; and it is confirmed that mental health will attend the planned MDT meeting.KE29. B is now self-neglecting and an increase in his care package is considered. The adult social worker had a face-to-face visit with B, and there is a continuation of his high levels of distress. B’s overall appearance has deteriorated, his self-care and personal hygiene are not being attended to.
January 2021 – Following the mental capacity assessment regarding management of finances B is deemed able to manage his finances with staff support. Supported Living contacted the GP and FRS to raise concerns of B expressing explicit suicidal thinking, namely jumping off the top of accommodation.KE30 The adult social worker was informed, and it is documented by them that it is not known what else the adult social worker can do. The adult social worker made a referral to the GP with these concerns. The risk of harm is escalating, but the trigger to deterioration is unknown. Staff lock the doors to the top floor as a precaution. FRS agree to contact B on his mobile and guidance is requested from MHAT. The GP and supported living are informed that B is open to social care and not mental health. Mental health IMR records that on 5th January the adult social worker advised that this was a mental health issue and not a social care one, therefore B needed to be referred back into mental health services, this was noted in social care IMR as urgent. Supported living then made a safeguarding referral due to concerns about suicide, this was triaged for the adult social worker to review under risk management.KE31 FRS contacted B who disclosed thoughts of suicide today, “he could not cope, and was going insane”. “I am continuously counting, and the numbers are doing my head in, I think I’m having a breakdown”. B is unable to identify any enjoyment, “feeling scared, everything is getting on top of me, talking doesn’t help”. When asked about harming himself B replied he was not going to but “didn’t know how he felt about ending his life at present”, which was a past response.KE32 B was not sleeping due to ongoing sexual thoughts, he cannot recall what medication he is on and states it was not helping, his communication was slow with long silences. FRS contact numbers are texted to B for use during the night. On 6th Jan 06:19hrs B called FRS with ‘busy thoughts’, ‘hard to think positively’. B said he did not know about harming himself when asked. He stated “I went upstairs in the building, I’m having a crisis and going insane’. B was unable to explain the crisis. Grounding techniques were attempted, and B terminated the call. 08:09hrs, B was contacted by FRS. “everything is worrying me…it feels like it is getting worse every day…thoughts about suicide…felt like this his whole life and wouldn’t act on them”. B agreed to talk to supported living… FRS informed the MHAT and supported living of contact with B. MHAT replied that B was not open to the team.KE33 FRS contacted B to ask if he wanted to be referred. B told GP that talking to FRS was not helping. The GP made a referral to CMHT (6th Jan), and the GP sent an email to the mental health single point of access (SPOA) with patient summary for this referral. On 6th Jan the mental health SAR (SAR appendix 2) recorded that adult social care advised mental health, that B should not be managed by social care, and he required a service from mental health. On 7th Jan – MHAT emailed FRS re the referral to advise that there was no change, but acknowledged B was more distressed.KE34 B saw the GP, who records that B was developing severe anxiety and panic, and B disclosed his negative thoughts. The GP recorded B was awaiting CMHT input. FRS record that B’s case is closed to mental health. The adult social worker had convened a multi-agency meeting with MHAT in attendance for January 22nd, to review what resources were available to meet B needs.KE34.1 B contacted FRS to inform them that he had told supported living staff he was going to make an attempt on his life.KE35 During a telephone consultation with the GP B was not relaxed, he was seeking reassurance. B stated, “I feel I am going insane; thoughts are getting worse”. On 8th Jan the GP records that the CMHT referral was rejected. In the referral outcome letter, there is advice is given to GP about PRN medication for anxiety.KE36 On 12th Jan B contacted FRS, he said he feels he is going insane, he had intrusive images and thoughts, B said he was having a panic attack, but breathing was determined by FRS as normal. FRS recorded the presenting situation in a letter to the GP, this included that counting numbers is part of his OCD, and this helps distract him.KE36.1 The letter notes that B was not expressing strange or abnormal beliefs.KE37 15th Jan – B spoke to the GP about his intrusive thoughts and that he was finding it difficult to distract himself. The GP advised B to go outside in the fresh air, to get some exercise, and to try listening to bird song, but B declined this advice and agreed to get in touch if he changed his mind. On 18th Jan, the advocate chased the complaint outcome, the complaint is acknowledged, and in response the consultant psychiatrist was to review the case before a response could be made.KE38 On 19th Jan 2021 Adult B died after jumping from the accommodation building. The meeting set for 22nd January 2021 is cancelled due to his death.
KE1 significant level of despair disclosed Aug 2019
KE2 statements about suicide in Aug 2019
KE3 B not monitoring blood sugar levels – management of diabetes Feb 2020 – is this a factor in his mental health deterioration?
KE3.1 is oesophagitis related to excess alcohol use disclosed in 2019, and does this physical illness further impact on B diabetes management?
KE4 assumption made that distress and anxiety is related to police investigation – yet his deterioration started before police enquiry. Images on the computer is a distraction for services – B needed mental health intervention.
KE5 what B reports in assessment is the opposite to the outcome of the assessment – no acute mental health.
KE6 package of care a major distractor in risk assessment and urgency of care need.
KE7 online and community resources details given to B is inconsistent to the concern about his limited cognitive ability to engage in services.
KE8 statement of intent of suicide with method identified. – high risk factor.
KE9 missed opportunity for review of B by consultant psychiatrist, B is not seen as having a relapse in mental health, consideration of diabetes and mental ill health not mentioned.
KE10 The mental health IMR provided to the SAR states that HTT clinicians concluded during a multidisciplinary meeting that B was not experiencing acute mental ill-health and he was not a risk to himself or others, this does not fit the information in April 2020
KE11 No psychotic or delusional symptoms were elicited at point of discharge and B was referred onto CMHT and on waiting list, this suggests B mental health had deteriorated and he had been acutely unwell, otherwise referral to the CMHT would not be appropriate. This appears contradictory to IMR information.
KE12 B is unable to engage in structured work the CMHT can provide, was there any consideration that talking about events triggers his own trauma?
KE13 where did possible diagnosis of autism come from, adult social care are not aware of this?
KE14 CRHTT involvement has improved his mental health presentation. B was less distressed and agitated, missed opportunity for follow up monitoring and support to supported living.
[42] Devon and Cornwall Police – A ViST form is submitted whenever a police officer identifies a person (adult or child) with care or support needs and / or is at risk of abuse or exploitation. This ViST is then graded green, amber or red. Red, amber and 3 green ViSTs in 3 months (escalating concern) are reviewed by the CST (Central Safeguarding Team) who conduct and include additional relevant research and decides if the additional information needs to be shared and with whom.
KE15 increase in suicidal thoughts disclosed.
KE16 missed opportunity to consider safeguarding discrimination and or neglect and there is no safeguarding escalation policy until Oct 2021
KE17 adult B is consistent with his thoughts about suicide and mental health deterioration now in July 2020, ongoing since August 2019.
[44] Stop it Now confidential helpline on 0808 1000 900, use our live chat or send a secure email, Confidential online self-help for anyone worried about their own sexual thoughts, feelings and behaviour towards children. Advice if you’re worried about another adult’s online or offline sexual behaviour towards children Help if you’re concerned about a young person’s sexual behaviour, Information on how to keep children safe from sexual abuse on our Parents Protect website and learning programme
KE18 conflicting information, considered not able to engage in taking therapies, yet able to access other services that would require B to engage in discussion and work.
KE19 B does have a forensic history, but he does not have any convictions. He disclosed he abused his sister and a child to police who investigated, no charges were brought as victims did not want to make complaint. There is no flexibility in services despite distress and concern about risk to children, this is not multi agency working.
KE20 pressures on services likely reason why assessment is not brought forward, 25 days before multi agency meeting – this does not address the GP concerns, no plan or specified intent is also influencing factor.
KE21 – no flexibility in the system due to pandemic- B needs not addressed
KE22 How clearly was this communicated as GP email “…finding solutions. I am hopeful that B should be considered for urgent therapy and support to manage his frustrations that all have a sexual theme….”
KE23 staff, police and GP all have concerns, GP and staff cannot do anything more, unclear how this is protective factor, mental health crisis and placement breakdown.
KE24 thoughts about sexual activity with children is a distraction, there is a mental health relapse and placement breakdown.
KE25 trauma, relapse in schizophrenia not considered, mental health team distracted by harming children,
KE26 unknown if diabetes and mental health deterioration are considered and followed up.
[45] Paramedics can work in GP surgeries and have their own clinics within the surgery. They manage a variety of presenting complaints and conduct urgent home visits to assist with GP workload. As part of a team, they work with other healthcare professionals and have their own area of responsibility. They can provide care independently and assess patients with symptoms and conditions such as suspected fractures or chest pain.
KE27 Supported living feel apathetic about requesting mental health for support and anticipating that none will be offered, this was echoed in the IMR and in interviews.
KE28 Is walking out into the road with moving traffic and lying down acting on thoughts of suicide?
KE29 attending a meeting is not addressing B need, his mental health continues to deteriorate.
KE30 consistent thoughts about suicide, method planned, attempt to go to upper floor prevented by staff, B made statement of intent.
KE31 this is a missed opportunity to consider discrimination or neglect under safeguarding to start escalating the concerns.
KE32 escalation in distress, statement of intent, acting on thoughts – this is different when seen with all information together, method tried.
KE33 – this is not accurate, B is not open to adult social worker and SW is unable to do anymore.
KE34 unclear why mental health do not think the situation has changed – it is acknowledged that B is more distressed.
KE34.1 this does not address the urgency multi agency meeting is 15 days away.
KE35 B is making a statement of intent to end his life
KE36 GP made referral shortly before B death to CMHT, which is later rejected – the referral is not a request for guidance.
KE36.1 this is information the GP already has – it does not provide solution focused action and number counting does not distract B, it increases his levels of distress, as this is a hierarchy of thoughts of actions of harm, there was no assessment of this in connection with voices.
KE37 B not expressing strange belief is not accurate as he is telephoning FRS he will make an attempt on his life and he has already identified the method, this is high risk.
KE38 unknown why complaint has taken two months or what consultants view was.
Appendix 5
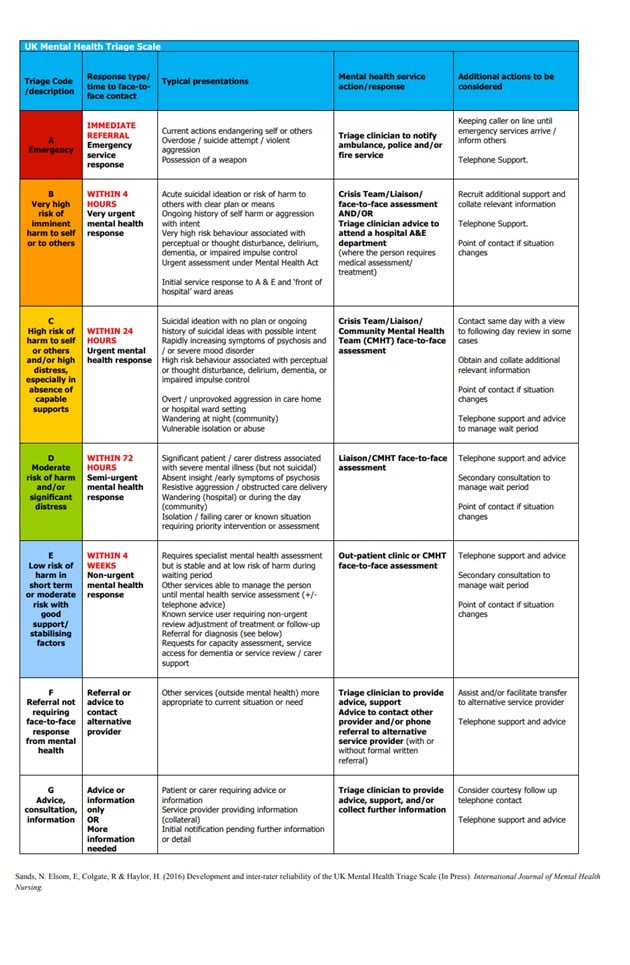
Appendix 6
SCIE SAR QUALITY MARKERS
SAR Quality Markers are a tool to support people involved in commissioning, conducting and quality-assuring SARs to know what good looks like. Covering the whole process, they provide a consistent and robust approach to SARs. In April 2022 SCIE relaunched the Safeguarding Adult Review (SAR) Quality Markers. First published in 2018, they have now been refreshed and updated.
The Quality Markers (QM) are based on statutory requirements, established principles of effective reviews and incident investigations, as well as practice experience and ethical considerations.
The SAR Quality Markers assume the principles of Making Safeguarding Personal, as well as the Six Principles of Safeguarding that underpin all adult safeguarding work (Empowerment; Prevention; Proportionate; Protection; Partnership; Accountable). These principles therefore permeate the Quality Markers explicitly and implicitly.
The SAR Quality Markers are intended to support commissioners and lead reviewers to commission and conduct high-quality reviews. They capture principles of good practice and pose questions to help commissioners and reviewers consider how they might best achieve them.
The SAR Quality Markers are arranged in three sections:
SETTING UP THE REVIEW
QM 1 Referral: The case is referred for consideration for a SAR with an appropriate rationale and in a timely manner.
QM 2 Decision making, What kind of SAR: Factors related to the case and the local context inform decision making about whether a SAR is required and/or desired and initial thinking about its size and scope. The rationale for these decisions is clear, defensible and reached in a timely fashion.
QM 3 Informing person, family and social network: The person, relevant family members, friends and network are told what the Safeguarding Adult Review is for, how it will work and the parameters, and are treated with respect.
QM 4 Clarity of purpose: The Safeguarding Adult Board (SAB) is clear and transparent, from the outset, that the Safeguarding Adult Review (SAR) is a statutory learning-focused process, designed to have practical value by illuminating barriers and enablers to good practice, untangling systemic risks, and progressing improvement activities. Any factors that may complicate this goal are openly acknowledged.
QM 5 Commissioning: Strategic commissioning of the Safeguarding Adult Review takes into account a range of case and wider contextual factors in order to determine the right approach to identifying learning about what is facilitating or obstructing good practice and/or the progress of related improvement activities. Decisions are made by those with delegated responsibility in conjunction with the reviewers, and balance methodological rigour with the need to be proportionate.
RUNNING THE REVIEW
QM 6 Governance: Safeguarding Adult Board (SAB) governance arrangements for the Safeguarding Adult Review (SAR) are sound, enabling defensible decision making, reliable over-sight and accountability regarding the SAR process, outputs and impact. The SAR achieves the requirement for independence and ownership of the findings by the SAB and member agencies and enables public accountability for learning and improvement.
QM 7 Management of process: The Safeguarding Adult Review (SAR) is effectively and considerately managed. It runs smoothly, is concluded in a timely manner and within available resources. The welfare of all participants is attended to. The process strives to help bring resolution to any tensions or conflicts between individuals or agencies as well as questions of families.
QM 8 Parallel processes: Where there are parallel processes taking place, the SAR is managed with the cooperation and communication required to avoid, as much as possible, duplication of effort, prejudice to criminal trials, unnecessary delay and confusion to all parties, including staff, the person and relevant family members.
QM 9 Assembling information: The Safeguarding Adult Review (SAR) gains a sufficient range and quality of information and input, to determine the relevant objective facts, to ‘stand in the shoes’ and ‘get inside the heads’ of those involved and to grasp the way that single and multi-agency/professional practice is shaped both by work environments and conditions, and by social and organisational factors. The kinds of data assembled allows unique versus generalisable issues to be distinguished. The extent of, and methods for, data gathering are transparent and proportionate to the practical value of the SAR.
QM 10 Practitioners involvement: The Safeguarding Adult Review (SAR) is informed by the experiences and perspectives of practitioners and managers, as relevant to the precise form and focus of the SAR commissioned. The process enables practitioners and managers to have a constructive experience of taking part in the review that helps cultivate an open learning culture.
QM 11 Involvement of person, relatives, family and network: The Safeguarding Adult Review (SAR) is informed by the person, relevant members of their family and social network in terms of information they hold, their experiences and perspectives as relevant to the precise form and focus of the SAR commissioned. The process enables the individual and family to see how the SAR is designed to have impact and contribute to positive change.
QM 12 Analysis: approach and methodology agreed for the SAR is used with optimum rigour within the size and scope of SAR commissioned. Analysis assumes a systems approach to safety and organisational reliability. It is anchored in relevant research and wider evidence base regarding effective clinical/professional practice and that of safety science. It draws on the full range of relevant information and input assembled, to evaluate and explain professional practice in the case(s) or the responses to earlier learning. Conclusions are of practical value, evidencing the wider learning identified about routine barriers and enablers to good practice, systemic risks and/or what has facilitated or obstructed change to date. There is transparency about any methodological limitations and the implications for the comprehensiveness or level of confidence in the analysis and findings.
OUTPUTS, ACTION AND IMPACT
QM 13 The Report: The length and detail of the SAR report match the size and scope of what was commissioned. As a minimum, it makes visible, in a clear, succinct manner, the systemic risks to the reliability of single and multi-agency safeguarding work that the SAR analysis has evidenced, in order to have practical value in directing improvement actions. It is written with a view to being published. Details of the person are included as judged necessary to illuminate the learning and/or in line with the wishes of the individual or their family.
QM 14 Publication and dissemination activities are timely and publicise the key systemic risks identified through the SAR, as well as features supporting high reliability of single and multi-agency working relevant to safeguarding. Compelling and engaging means of circulating the findings are used, adapted as necessary for different operational and strategic audiences. Decisions about what, when, how and for how long to publish and disseminate findings are made with sensitive consideration of the wishes and impact on the person, family and other families; professionals who participated are kept informed and supported as needed. Publication and dissemination foster active responsibility and public accountability for addressing barriers identified to good practice or progressing improvement work.
QM 15 Improvement action and evaluation impact – Improvement actions agreed in response to the SAR set ambitious goals, seeking to align the motivations of different stakeholders, bringing partners together in new ways and foster collaborative working. Actions are integrated, wherever possible, with wider strategic improvement activity, plans and priorities, led locally, regionally or nationally. Evaluation of impact is designed from the start, supported by a logic model or similar, using measures that demonstrate whether the underlying causes of systemic risks identified have been addressed. The SAB maintains a public record of findings, actions and commentary to enable public accountability.
Appendix 7
INTERVIEWS HELD FOR THIS SAR
Family member Adult C
Family member Adult N – telephone enquiry, request for an opportunity be involved with outcomes.
Supported living staff x 3
Adult social Worker
Supported Living Senior Manager and Registered Manager
Mental health Legal Officer for Safeguarding and Public Protection
Deputy Director of Nursing and Allied Health Professions – Patient Safety
LR attendance at an inquest via video link in late January 2023 heard evidence presented by staff directly involved. Emergency department and psychiatric liaison
First Response Operational Service Manager
Deputy Director, Safeguarding & Public Protection
Appendix 8
LEAD REVIEWER BIOGRAPHY
The Lead Reviewer commissioned for this SAR has relevant experience to undertake a themed review. The reviewer has a professional background in mental health, learning disability, forensic psychiatry, and education, with thirty plus years working in statutory services and multi-agency partnerships, and from 2002 in senior safeguarding roles. After leaving statutory services the reviewer has worked as an independent reviewer and safeguarding consultant.
Experience includes clinical and managerial positions, significant safeguarding and public protection experience, direct work with victims /survivors of abuse and police as a specialist interviewer. The LR has completed trauma awareness and the trauma continuum training and has many years’ experience of working with individuals with complex trauma.
The LR has experience of undertaking clinical incident reviews, complaints, SARs, child protection reviews, mental health homicides, domestic abuse homicides (DHR) as internal IMR author and an overview report author, DHR and Mental Health Homicide panel member and panel chair. The LR is an accredited SCIE Learning Together reviewer (systems reviews).